Deciding on the Right Treatment
- Actress Olivia Munn, 43, was diagnosed with breast cancer despite receiving a ‘normal’ mammogram and testing negative for the BRCA gene mutation, which increases your cancer risk. Amid treatment, which included a double mastectomy (removal of both breasts) and breast reconstruction, she also underwent a full or total hysterectomy.
- A hysterectomy is a procedure that removes part or all of the uterus (or womb), often along with the cervix, according to the National Cancer Institute. Women who receive a diagnosis of uterine, ovarian, and cervical cancer may have their cancer treated with a hysterectomy.
- A side effect of a hysterectomy is infertility. However, cancer patients wishing to have children can preserve their fertility by freezing eggs for use through in vitro fertilization (IVF).
Actress Olivia Munn, 43, is hopeful she’s finally done with surgeries related to her breast cancer diagnosis after undergoing a full hysterectomy. The procedure removed all of the uterus (or womb) along with the cervix.
Though the “New Girl” star has taken steps to improve her cancer diagnosis, it came with a risk. The 43-year-old actress and mother of one wants to keep her options open for another child. However, a hysterectomy eliminates the chance of conceiving pregnancy. Fortunately, she froze her eggs, making in vitro fertilization (IVF) surrogacy an option.
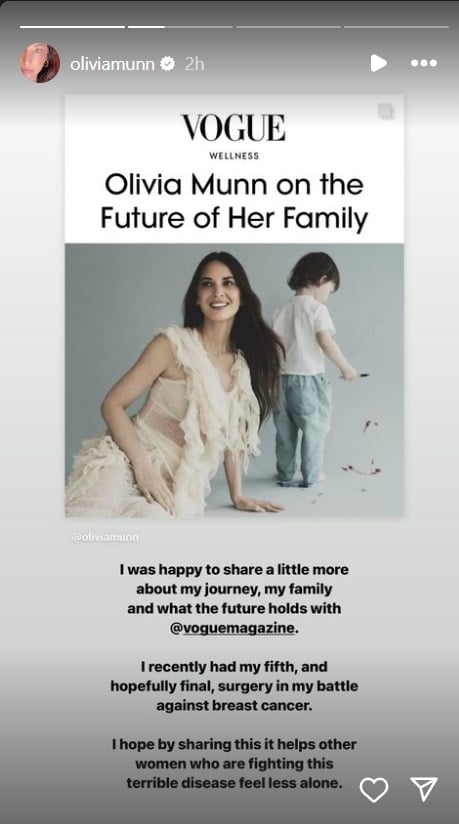
“I took out my uterus, fallopian tubs, and ovaries,” Munn told Vogue.
The actress noted how odd it felt to suddenly stop having periods after the procedure.
“It’s just so strange when you’ve been with this body your entire life, had your period for so long, feel when you’re ovulating, and all of a sudden it’s gone,” Munn said.

The flip side of a hysterectomy is its impact on fertility. Munn had been freezing her eggs because she knew her cancer treatment could impact her fertility. She said as she inched closer to 40, her eggs were becoming less viable.
“As you get older, one month can have great eggs, the other not so much. Clearly, the month we did at 39 was not a good month. After my diagnosis, we decided to try one more round of egg retrievals and hope it was a good month,” Munn explained.
Munn was able to have two healthy embryos in the event she and her partner wished to have another child. When the doctor called her with the news, Munn said she started crying.
“It was just so exciting because not only did we get it in one retrieval, but it meant that I didn’t have to keep putting myself at risk. It was just amazing,” Munn said.
Expert Resources on Breast Cancer Treatment Options
- ‘Real Housewives’ Alum Vicki Gunvalson Says Cancer Cells Not A Cancer Diagnosis Led to Her Full Hysterectomy
- For Breast Reconstruction After Mastectomy, Women May Choose ‘Now,’ ‘Later,’ or ‘Never’
- Is a Preventative Mastectomy Right for Me?
- Implant Reconstruction After a Mastectomy: The Options
- Should I Have a Lumpectomy or Mastectomy?
How a Hysterectomy Impacts Cancer Treatment and Fertility
A hysterectomy is a procedure that removes part or all of the uterus (or womb), often along with the cervix, according to the National Cancer Institute. Women who receive a diagnosis of uterine, ovarian, and cervical cancer may have their cancer treated with a hysterectomy.
Women may need a hysterectomy for a variety of reasons she and her doctor carefully review. Some examples may include endometrial cancer, ovarian cancer, endometriosis, chronic pelvic pain or vaginal bleeding, and uterine fibroids.
In a previous interview with SurvivorNet, Dr. Heidi Gray, a gynecologic oncologist, discussed open versus robotic surgery and how the two can be used to perform a hysterectomy.
“The most common procedure that we do robotically would be a hysterectomy, removal of the tubes and ovaries, you can also do more complicated omentectomy removing of the omentum [a fatty apron surrounding abdominal organs],” Dr. Gray explained.
The National Cancer Institute explains that there are different types of hysterectomy procedures.
- Total hysterectomy: Removal of the uterus and cervix, but the ovaries and fallopian tubes may also be removed.
- Supracervical hysterectomy: Removal of just the upper part of the uterus but keeping the cervix. This may also be called a partial hysterectomy.
- Total hysterectomy with bilateral salpingo-oophorectomy: Removing the uterus, cervix, fallopian tubes (salpingectomy), and ovaries (oophorectomy).
- Radical hysterectomy with bilateral salpingo-oophorectomy: Removing the uterus, cervix, fallopian tubes, ovaries, the upper portion of the vagina, and some surrounding tissue and lymph nodes. This hysterectomy is done when cancer is involved.
Fertility Preservation Options for Cancer Patients
Certain types of chemotherapy can destroy eggs in your ovaries. This can make it impossible or difficult to get pregnant later. Whether or not chemotherapy makes you infertile depends on the drug type and age since your egg supply decreases with age.
“The risk is greater the older you are,” reproductive endocrinologist Dr. Jaime Knopman told SurvivorNet.
“If you’re 39 and you get chemo that’s toxic to the ovaries, it’s most likely to make you menopausal. But, if you’re 29, your ovaries may recover because they have a higher baseline supply,” Dr. Knopman continued.
Radiation to the pelvis can also destroy eggs. It can damage the uterus, too. Surgery to your ovaries or uterus can hurt fertility as well.
Meanwhile, endocrine or hormone therapy may block or suppress essential fertility hormones and may prevent a woman from getting pregnant. This infertility may be temporary or permanent, depending on the type and length of treatment.
If you have a treatment that includes infertility as a possible side effect, your doctor won’t be able to tell you whether you will have this side effect. That’s why you should discuss your options for fertility preservation before starting treatment.
WATCH: How chemotherapy affects fertility.
Research shows that women who have fertility preserved before breast cancer treatment are more than twice as likely to give birth after treatment than those who don’t take fertility-preserving measures.
Most women preserve their fertility before cancer treatment by freezing their eggs or embryos.
After you finish your cancer treatment, a doctor specializing in reproductive medicine can implant one or more embryos in your uterus or the uterus of a surrogate with the hope that it will result in pregnancy.
If you freeze eggs only before treatment, a fertility specialist can use sperm and eggs to create embryos in vitro and transfer them to your uterus.
When freezing eggs or embryos is not an option, doctors may try these approaches:
- Ovarian tissue freezing is an experimental approach for girls who haven’t yet reached puberty and don’t have mature eggs or for women who must begin treatment immediately and don’t have time to harvest eggs.
- Ovarian suppression prevents the eggs from maturing so they cannot be damaged during treatment.
- For women getting radiation to the pelvis, Ovarian transposition moves the ovaries out of the line of treatment.
In addition to preserving eggs or embryos, positive research has shown that women with early-stage hormone-receptor (HR) positive breast cancer were able to safely pause endocrine therapy (ET) to try to get pregnant, and they did not have worse short-term recurrence rates than people who did not stop endocrine therapy.
Olivia’s Breast Cancer Journey
Munn’s breast cancer diagnosis emerged despite receiving a “normal” mammogram and testing negative for the BRCA-gene mutation, which increases your risk for breast and ovarian cancer.
At the suggestion of her OBGYN, the “X-Men” actress underwent a Breast Cancer Risk Assessment, which helps determine a woman’s probability of getting breast cancer. Her results called for additional screening, which revealed she had an aggressive form of cancer in both of her breasts.
“I wouldn’t have found my cancer for another year – at my next scheduled mammogram – except that my OBGYN…decided to calculate my Breast Cancer Risk Assessment Score. The fact that she did save my life,” Munn said in an Instagram post.

The Breast Cancer Risk Assessment she credits for catching her breast cancer is a “statistical model that allows healthcare professionals to calculate the probability of a woman developing breast cancer over the course of their lifetime,” Dr. Ruth Oratz, breast medical oncologist, NYU Langone Health’s Perlmutter Cancer Center; clinical professor of medicine, NYU Grossman School of Medicine tells SurvivorNet.
Munn underwent genetic testing to better understand her cancer risk.
Genetic tests can be as simple as a simple saliva swab or blood sample. The results help your care team determine if you have a specific mutation that puts you at higher risk for cancer. The results help doctors tailor your treatment and are helpful for breast cancer patients.
“I tested negative for all (different cancer genes), including BRCA,” Munn said.
The BRCA1 and BRCA2 gene mutations are among the most important genes to look for in breast cancer. Together, they are responsible for about half of all hereditary breast cancers. These genes prevent cells from dividing haphazardly and uncontrollably in a person without mutations. Mutations prevent these genes from doing their job and can allow unchecked growth of breast, ovarian, and other tissues.
Two months after undergoing genetic testing, Munn was diagnosed with Luminal B breast cancer in both of her breasts.
According to research in “Breast Cancer,” luminal B tumors are of a “higher grade” and tend to have a worse prognosis. This type of breast cancer is estrogen-positive (ER), meaning it is fueled by the hormone estrogen. It can also be progestogen (PR) negative, meaning it is not fueled by progestogen. This type of breast also tends to have a higher expression of the Ki67 protein, making it grow quickly. Hormonal therapy and chemotherapy are often used to treat this type of cancer.
Luminal is one of several types and is distinguished by its molecular makeup. Other types of breast cancer types include:
- Luminal A breast cancer
- Luminal B breast cancer
- Luminal B-like breast cancer
- HER2-enriched breast cancer
- Triple-negative or basal-like breast cancer
Each type has a specific, individualized molecular structure. The different types of breast cancer’s molecular structure may inform the treatment path.
Olivia’s Cancer Treatment
Munn underwent a double mastectomy to treat her cancer.
When a woman decides to have a mastectomy, several factors go into that decision. Among things to consider is whether to have breast-conserving surgery such as a lumpectomy. These decisions should be made alongside your doctor by openly and candidly discussing risks vs. benefits.
“A double mastectomy typically takes about two hours for the cancer part of the operation, the removing of the tissue,” Dr. Elisa Port, Chief of Breast Surgery at Mount Sinai Health System, tells SurvivorNet. “The real length, the total length of the surgery, can often depend on what type of reconstruction [a patient] has.”
WATCH: What Happens During a Double Mastectomy
Other factors that weigh into the decision to get a mastectomy are the size and features of the tumor and your family history. However, the gravity of your decision comes into full view, especially if you choose to get a mastectomy and remove both of your breasts.
Some women decide to have their breasts reconstructed and have implants put in right after the mastectomy, while others don’t have reconstruction at all.
Dr. Port added that most women opt to have some reconstruction. The length of these surgeries can vary greatly. When implants are used, the procedure can take two to three hours (so the total surgery time would be around five hours). There is also the option to take one’s own tissue (usually from the belly area) and transfer it into the breast area during reconstruction.
What To Ask Your Doctor
If you have been diagnosed with breast cancer, you may have questions about keeping your strength through treatment. Here are a few questions to help you begin the conversation with your doctor:
- What treatment will I be receiving?
- What side effects are associated with this treatment?
- Are there steps I can take daily to help minimize these side effects?
- What physical activity routine do you recommend for me during treatment?
- Do you have recommendations for someone who doesn’t particularly enjoy exercise?
- Can you recommend a dietician who can help me with healthy eating tips and weight maintenance?
- I’ve been having trouble sleeping. Do you have any treatment recommendations?
Learn more about SurvivorNet's rigorous medical review process.

