Milestones After Beating Cancer
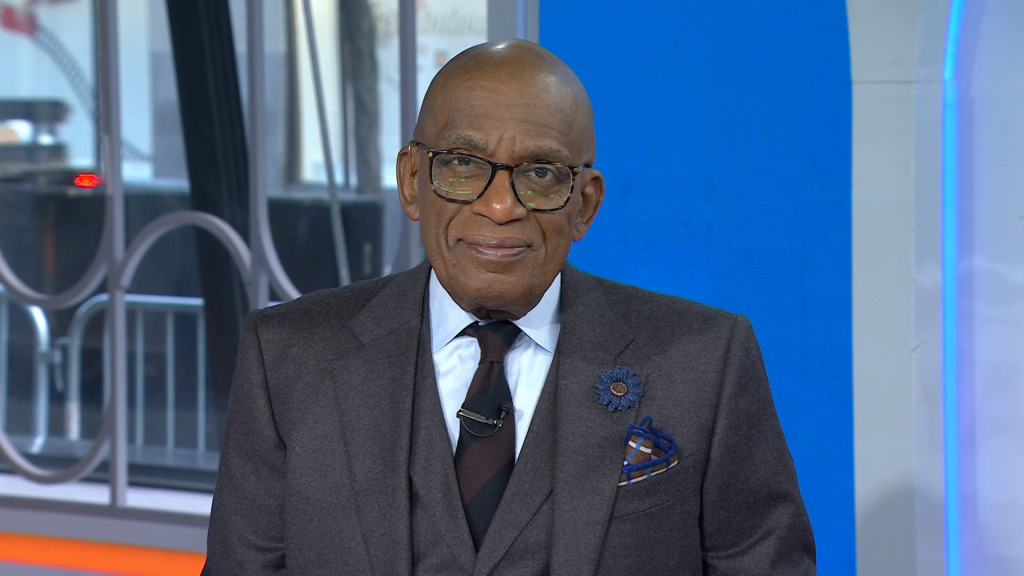
- Today co-host Al Roker is recounting his personal health story as he celebrates a very special Father’s Day this year as a new “pop-pop,” or grandpa to his granddaughter, Sky.
- The beloved weatherman was diagnosed with prostate cancer in 2020 after a routine PSA screening, a prostate-specific antigen (PSA) test. This test measures the level of PSA in the blood, and higher levels can indicate cancer.
- Roker underwent surgery one month later, but it’s important to know that not all men diagnosed with prostate cancer require surgery, with doctors instead, using active surveillance, a “watch-and-wait” approach for less aggressive cases.
- Prostate cancer screening guidelines released this year now urge Black men to begin screening at 40 years old, which is 10 to 15 years earlier than men at average risk. The National Cancer Institute says among Black men, “death rates are higher” or “more than twice” that of white men, sparking increased efforts to boost early detection for this demographic.
- SurvivorNet holds an annual Close the Gap conference to educate, spread awareness, and ultimately work to eliminate racial disparities in cancer care. Our efforts aim to ensure everyone has access to education about cancer, screening recommendations, treatment options, clinical trials, and more.
“I’m so grateful I’m here to be able to see my first grandchild,” the beloved weatherman, 69, shared in a personal essay with PEOPLE, speaking of his eldest daughter Courtney’s little girl, Sky, 11 months.
Read MoreLast week, Roker posted an Instagram reel of the duo spending time together, which was set to Natalie Cole’s “This Will Be (An Everlasting Love).”
“My Girl!!” he wrote.
View this post on Instagram
Elsewhere in Roker’s latest essay, he gushed that he just loves spending time with Sky.
“She’s well-loved. She’s a very content baby.”
The well-known foodie also noted that this granddaughter “has a very good palate,” and just last weekend, was eating some anchovies, olives and grapefruit from his salad.

“She likes savory very much,” he added. “That’s not surprising because her mom is a chef.”
Al Roker’s Prostate Cancer Diagnosis
Delving into more serious details of how he found out about his cancer, Roker said he had initially almost put off his routine physical but finally had a “lull” in his busy schedule during COVID.
Soon after, Roker’s medical team alerted him that his PSA, or prostate specific antigen, was up. The test detects it in the blood.
They decided to retest. Still no change. Roker was told they needed to do a biopsy. It was then that he received his diagnosis.
“To be perfectly honest, I don’t really remember what he said. I heard ‘prostate cancer’ and then I zoned out, which goes to the point that it always helps to have somebody there with you,” he shared, adding “it was all just a blur.”
Roker did remember being told it could be “somewhat aggressive.”
When he went home to tell Roberts, “after the initial shock,” he said that Deborah “was alarmed.”
“She was obviously worried. She said, ‘I must look like a terrible wife. I wasn’t there for you when you needed me.’ But how could I tell her? I didn’t know.”
Instantly, Deborah “went into full advocacy mode,” handling appointments and taking notes and “all that stuff.”

“She was so thrilled that she was there to do it.”
One month later, Roker underwent surgery at NYC’s Memorial Sloan Kettering to remove his prostate, lymph nodes and surrounding tissue.”
Pushing for Earlier Screenings of Prostate Cancer
Prostate cancer is the most common type of cancer in males, typically affecting 1 in 8 during their lifetime.
Since his cancer journey, Roker has become a strong voice in the cancer community, pushing men to get in for screenings, especially Black men, who have a higher death rate from the disease.
Staggeringly Higher Prostate Cancer Rates for Black & Latino Men
According to research published in the World Journal of Men’s Health, in the U.S., cases of prostate cancer among Black men are “60 percent higher” than white men.
Prostate cancer does not always behave the same in every man it impacts. The cancer can be considered “low-risk” and can be slow-growing, and treatment might not be necessary.
In other men, the cancer may grow faster or more aggressively, requiring more immediate treatment. Because of this, there is some debate about screening.
Screening Guidelines
The United States Preventive Services Task Force recommends men at average risk between the ages of 55-69 years old should talk with their doctor about the pros and cons of prostate cancer screening.
The American Cancer Society recommends that men at age 50 who are at average risk should begin screening. Men who are at high risk of prostate cancer, including the Black community, should begin screening at age 40, while men with a close relative diagnosed with prostate cancer should consider annual screenings in their 30s.
Black Americans Need to Prioritize Cancer Screenings, Says Leading Radiation Oncologist
Most doctors agree that men over the age of 70 do not need screening.
SurvivorNet experts suggested that men consider factors like their family history, genes, and age when deciding whether and when to screen.
Symptoms of prostate cancer may include:
- Urinating more often
- Waking up in the middle of the night to pee
- Blood in your urine
- Trouble getting an erection
- Pain or burning when you urinate
- Pain in your back, hips, thighs, or other bones
- Unexplained weight loss
- Fatigue
How Is Prostate Cancer Staged?
The National Comprehensive Cancer Network (NCCN) guidelines divides prostate cancer into one of six risk categories based on how aggressive the cancer looks under the microscope and the chance of it coming back after treatment. These risk categories help guide treatment for the different subtypes of prostate cancers.
The main risk categories for prostate cancer are:
- Very-Low-Risk (VLR) and Low-Risk (LR)
- Favorable- (FIR) and Unfavorable-Intermediate-Risk (UFIR)
- High-Risk (HR) and Very-High-Risk (VHR)
Very-Low-Risk and Low-Risk Prostate Cancers
Prostate cancers classified as VLR or LR represent the least aggressive forms of cancer. This categorization will be diagnosed depending on number of factors, including:
- Your doctor can’t feel the cancer on a physical exam, or it occupies one-half or less of one side of the prostate
- Your PSA is less than 10
- Your total Gleason score is 6
- If your cancer is categorized as VLR or LR, your doctor may recommend active surveillance, another name for “watch-and- wait”
Who is a Candidate for Active Surveillance?
Not all men with prostate cancer are potential candidates for active surveillance. Active surveillance is only recommended for men with low-risk prostate cancer who are capable and willing to follow a very close and active follow-up schedule. Low-risk prostate cancer is slow growing and is biologically less aggressive compared with higher-risk prostate cancer.
“With low-risk prostate cancer, your risk of cancer getting out of the prostate and spreading to other parts of the body is really, really low,” Dr. Stephen Freedland, a urologist at Cedars-Sinai Medical Center, previously told SurvivorNet when discussing the topic.
Learning More About Active Surveillance
Men who have low-risk cancer can choose this approach and avoid the potential complications that come with treatment with surgery and radiation. Because the risk of the cancer spreading outside of the prostate is extremely low in men with low-risk disease, this approach is an effective option for men.
RELATED: People With Low-Risk Prostate Cancer Can Rely on Monitoring the Disease
Active surveillance includes a PSA test, rectal exam and high-quality imaging tests, which can identify minuscule yet important changes.
Questions for Your Doctor
If you have experienced symptoms associated with prostate cancer or have a screening coming up, here are some questions you may ask your doctor:
- If I have elevated prostate-specific antigen (PSA) levels, what could be causing that besides cancer?
- How long will it take to learn if my PSA levels warrant further testing?
- What are the treatment options that are best suited for me based on my risk level?
- What financial resources exist to help me with the costs associated with treatment?
- How long will my potential treatment prevent me from working or continuing normal activities?
Learn more about SurvivorNet's rigorous medical review process.

