Brain Cancer Awareness
- Brain cancer affects approximately 24,530 people annually in the U.S.
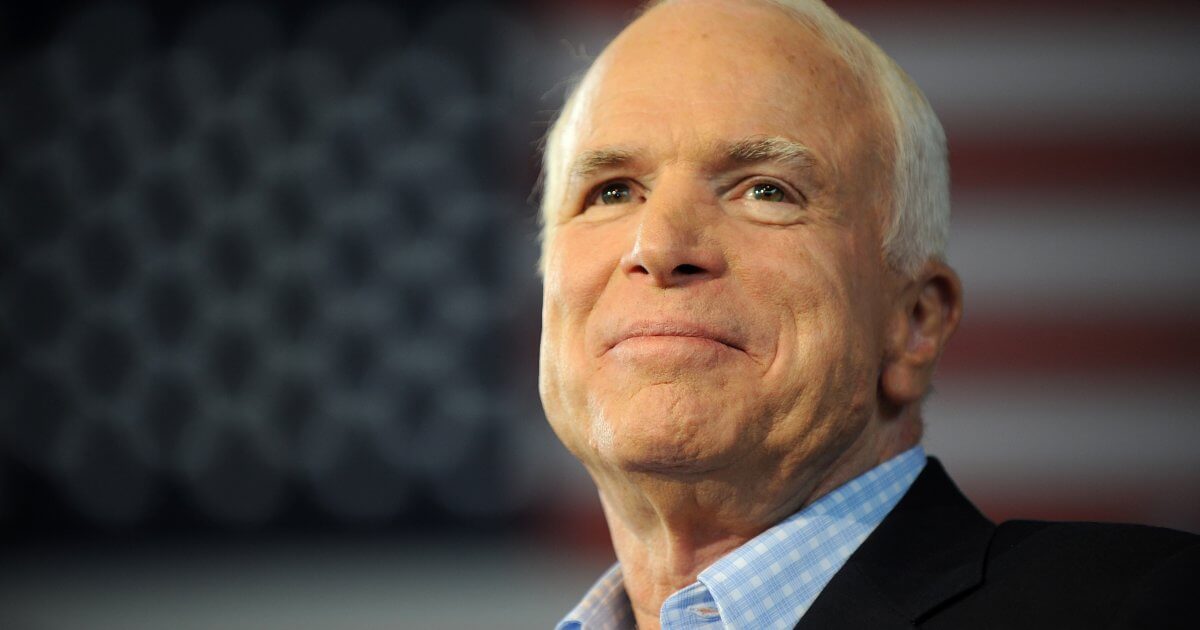
- Politicians John McCain and Ted Kennedy both passed away after battles with this disease.
- Treatment options for brain cancer include surgery, radiation, and chemotherapy.
Senators John McCain and Ted Kennedy both passed from brain cancer — McCain in 2018 and Kennedy in 2009. In 2015, President Joe Biden’s son Beau also died from the disease. Have treatment options changed significantly since then? SurvivorNet takes a look at recent advances in brain cancer.
Read MoreBiden, McCain & Kennedy’s Brain Cancer Battles
Senator John McCain underwent treatment for glioblastoma (GBM) brain cancer starting in July 2017, and he ended his treatment before passing in August 2018.
Senator Ted Kennedy’s brain cancer presented via a seizure in May 2008, which led to a diagnosis of a malignant brain tumor. He was told the cancer was inoperable, but that he could undergo chemotherapy and radiation. After getting a second opinion, however, Kennedy eventually had an operation at Duke University in June 2008.
At the time, Kennedy was told the procedure was successful, but Kennedy later worsened. He passed away in August 2009.
Could a New Treatment Have Saved John McCain? Fighting Brain Cancer With Electric Fields
Beau Biden was diagnosed with glioblastoma in 2013, and underwent surgery, chemotherapy and radiation for the disease. He was then able to go back to work as Delaware’s Attorney General. Sadly, the father of two suffered a recurrence the following spring, and his health turned quickly. Prior to his diagnosis, in 2010, the Iraq War Veteransuffered from a stroke, which luckily had been mild. There is no evidence whether this was a symptom of his brain cancer or unrelated.
New Options for Brain Cancer Treatment
Treatment options for brain cancer include surgery, radiation and chemotherapy. Some researchers are working to create broader treatment options for brain cancer like glioblastoma, the kind of cancer with which McCain and Kennedy were diagnosed.
Glioblastoma is the most aggressive primary brain tumor. But despite its aggressive nature, Duke University Medical Center’sDr. Henry Friedman says in an earlier interview there is hope. Dr. Friedman is a top brain researcher in the U.S., as well as a neuro-oncologist.
You are not dead just because you’re diagnosed with a glioblastoma, he says. So many people are told by their doctors or their institutions that they’re at, 'I’m sorry, put your affairs in order and just move on.’
Dr. Friedman and his Duke colleagues are investigating a new therapy that combines the modified poliovirus and immunotherapy. The modified poliovirus is used to treat this tumor, by injecting it directly into the tumor, through a catheter. It is designed to lyse the tumor and cause the tumor cells to basically break up he says.
I think that the modified poliovirus is going to be a game-changer in glioblastoma, explains Dr. Friedman, but I should also say that its reach is now extending into melanoma soon to bladder cancer.
When discussing the success of the poliovirus study, Dr. Friedman tellsSurvivorNet, It has helped a large number of patients, but not enough. We have a prolonged survival curve of about 18% going out many, many years in our initial trial. We don’t want to have 18%, 15%, 20% of people who are long-term survivors. We want them to be at a much higher number.
Dr. Friedman and his colleagues are now taking this a step further by combining this treatment with a type of immunotherapy, called acheckpoint inhibitor.Specifically, the Duke team is using a drug called pembrolizumab (Keytruda) and is coupling it with the modified poliovirus. By combining these therapies the study team hopes the GBM patient’s own immune system will be better equipped to attack and kill the cancer cells. While this is exciting, and certainly a point of hope for patients with GBM, this combination therapy needs to be tested in a clinical trial setting before it can be used to treat all patients with GBM. Currently, the researchers are working toward a clinical trial using the modified poliovirus with pembrolizumab for patients with recurrent GBM.
How Can Tumor Treating Fields Help Brain Cancer Patients?
Tumor-Treating Fields (TTFields) use low-intensity electric fields to disrupt the cell division process, making it harder for cancerous cells to multiply.
But what’s especially promising about TTFields is that they are not accompanied by the pain, nausea and fatigue that so often go along with chemotherapy and radiation therapy. And because TTFields are noninvasive treatments, the therapy doesn’t demand the same kind of recovery time as surgery. Another key benefit of TTFields? They are most effective against cancer cells, having relatively little impact on normal cells, according toDr. Wenyin Shi, co-director of the Brain Tumor Center of the Sidney Kimmel Cancer Center in Philadelphia.
RELATED: What Are Tumor Treating Fields?
TTFields only have non-overlapping toxicity with conventional anti-cancer treatments, but they also may enhance the efficacy of conventional treatment, says Dr. Shi, whose research has focused on optimizing TTFields treatment for patients with glioblastoma (GBM). I anticipate the utilization of TTFields will increase and may be as routinely used as other anti-cancer treatments.
TTFields is still a relatively new treatment option. It was developed by Novocure and is called Optune. The FDA first approved it to treatglioblastomain 2011, and thenapprovedit in 2019 to treat mesothelioma.
A large phase 3 randomized trial has proven the use of TTFields can markedly improve the overall survival of patients with newly diagnosed GBM, Dr. Shi says, adding that the National Comprehensive Cancer Network has given TTFields its level 1 recommendation (strongest endorsement based on scientific evidence) for newly diagnosed GBM patients. TTFields clearly is a new weapon for oncologists, says Dr. Shi, adding that the therapy has more than doubled the five-year survival rate for newly- diagnosed GBM patients.
Learn more about SurvivorNet's rigorous medical review process.