Fertility & Moving Forward After Cancer
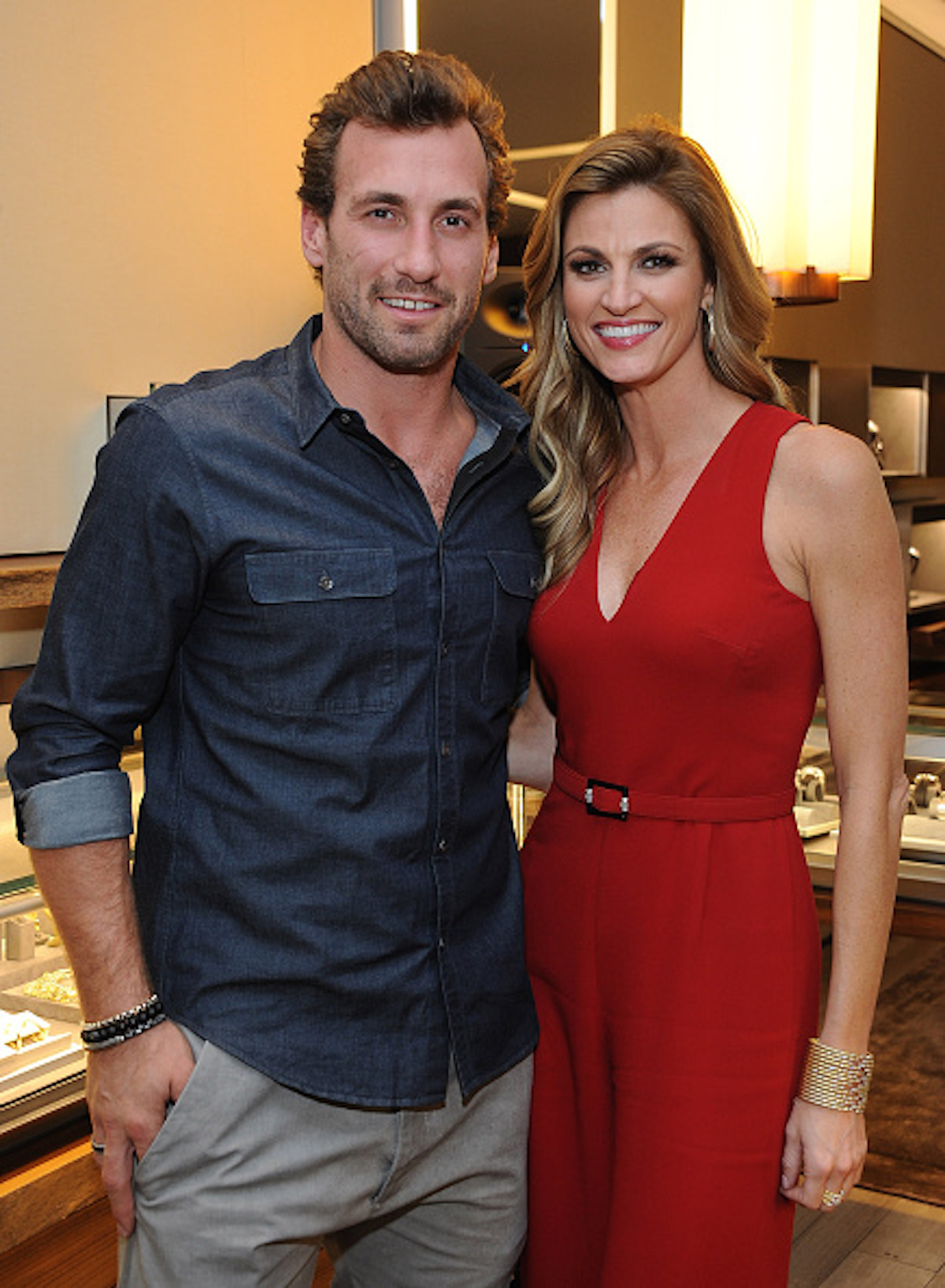
- Erin Andrews, who was diagnosed with cervical cancer during a routine screening in 2016 and treated the disease with surgery, has just welcome her first child into the world with her former NHL player husband Jarret Stroll.
- Cervical cancer begins in the cells lining the cervix the lower part of the womb (uterus). Treatment options for cervical cancer include surgery, chemotherapy and/or radiation therapy. HPV (human papillomavirus), a sexually-transmitted virus, causes more than 70% of cervical cancer cases.
- Doctors should bring up fertility preservation with every woman of childbearing age before she starts cancer treatment. In Andrews’ case, she and her husband had already had frozen embryos before her diagnosis.
- In some cases after cancer treatment, women may have difficulty giving birth to a child or they may be unable to at all. Having someone else carry their baby, like Andrews, may be an option, either through surrogacy or a gestational carrier.
The birth of their newborn baby boy was confirmed this week to TODAY.com and comes after an exhaustive journey through fertility and IVF treatments.

“For those familiar, you know it's a time-consuming and emotionally draining process. This is my 7th one, and I've been going through these treatments since I was 35 years old,” she continued.
Expert Cancer & Fertility Resources
- After A Cancer Diagnosis: Getting Fertility Hormone Injections
- Fertility Preservation After a Cancer Diagnosis
- How Does Chemotherapy Affect Fertility?
- Can I Have A Baby After Breast Cancer?
- New Evidence That IVF Is Linked To Higher Rates Of Breast Cancer– A Leading Expert Explains Why Women Shouldn’t Necessarily Be Alarmed
The then-43-year-old, said her body was “stacked against” her, adding, “I have been trying to do IVF treatment for a while now, but sometimes it doesn't go the way you want it. Your body just doesn't allow it.
“Every cycle is different in a woman's body, so some months are better than others.” Andrews said that the scheduling difficulties made her question what’s most important, leaving her feeling as if she needed to choose between family and a career.
Thankfully, she ultimately spoke with her producers and told them that she'd be late to work, due to daily fertility appointments, something she’s “thankful” she did. “They encouraged me to be open about it because this is real life. It's not like I'm leaving to go take a hot yoga class, I'm trying to have a baby. I am not ashamed, and I want to be vocal and honest about this.”
Prior to that, Andrews also opened up to Health in 2017 about how she previously had undergone IVF prior to her diagnosis.
“I had actually frozen my eggs before all this a couple of years back, just because it was all the rage. But it definitely took a serious turn for us. I'm not young, we don't know when we're gonna have a baby, we don't know if this is going to come back,” Andrews said.
“One thing I love my future husband for is that our oncologist said the smart thing to do would be to have some insurance waitingso we have frozen embryos because we've taken the steps. If we need 'em, we need 'em; and if we don't, we don't. We just wanna be smart. But it's crazy, because these waiting rooms are packed!”
As for how she will handle both her career and family, Andrews exuded confidence in her ability to balance it all.
She told Health, “For me, it's having the career, having the family, and having the happiness. I grew up in the South. People were getting married at 21; I had my first major job at 21, and I was missing everybody's weddings because I was doing football games and baseball games.
“I had never been to Europe until two years agoI've gone to all the sports cities, but I'd never had a life for myself. I want to continue doing more, but it's going to be shaped toward how I want to have this family and how I do want to have kids.
“I think it's possible that I'll be able to have a kid and be able to do this for a living. We're just gonna have to figure out how.”
Erin Andrews’ Cervical Cancer Battle
Andrews was 38 when doctors detected cervical cancer during a routine pap screening in 2016.
Since her diagnosis, Andrews has been a vocal advocate for women to stay current on their cancer screenings. To treat her cancer, Andrews underwent two surgeries.
Prior to surgery, she had In Vitro Fertilization (IVF) to preserve her fertility.

Cervical cancer is detected via a pap smear test, which looks for early signs of cervical cancer. Nurse Practitioner Barbara Dehn told SurvivorNet in an earlier interview, “Many women think that a Pap smear checks for ovarian cancer, but it doesn't. Pap smears detect only cervical cancer, not all gynecologic cancers.
“In fact, there is no test that detects ovarian cancer in its earliest stages, which is why two-thirds to three-quarters of women are diagnosed at a later stage, when the disease has spread to nearby tissues and organs.”
Every year in the U.S., approximately 11,500 women will be diagnosed with cervical cancer, according to the Centers for Disease Control and Prevention.
Getting pap smears to detect for cervical cancer is critically important because an earlier diagnosis may mean a better prognosis and broader treatment options.
Understanding Cervical Cancer
Cervical cancer begins in the cells lining the cervix the lower part of the womb (uterus). Treatment options for cervical cancer include surgery, chemotherapy and/or radiation therapy.
It’s important to note that HPV (human papillomavirus), a sexually-transmitted virus, causes more than 70% of cervical cancer cases.
Additionally, other risk factors like smoking can make you about twice as likely to get cervical cancer as those who don't smoke.
Cervical cancer screening is critically important because an earlier diagnosis can mean a better prognosis with broader treatment options.
The American Cancer Society recommends that cervical cancer screening begins at age 25, and people aged 25 to 65 should have a primary HPV test, an HPV test done by itself for screening, every 5 years. If primary HPV testing is not available, however, screening may be done with either a co-test that combines an HPV test with a Papanicolaou (Pap) test every 5 years or a Pap test alone every 3 years.
The most common symptoms of cervical cancer can include:
- Abnormal vaginal bleeding, such as bleeding after vaginal sex, bleeding after menopause, after douching, bleeding and spotting in between periods or having heavier or longer (menstrual) periods than usual.
- Unusual discharge from the vagina that may contain some blood and may occur between your periods or after menopause.
- Pain during sex.
- Pain in the pelvic region.
Understanding Fertility Preservation
“When a woman is diagnosed with cancer in her childbearing years, fertility preservation should be a part of the conversation, like it's part of the treatment plan,” Jaime Knopman, MD, a reproductive endocrinologist at CCRM Fertility in New York City, previously told SurvivorNet.
“Everyone in their reproductive years should be advised of their options.”
Freezing Eggs Or Embryos: What Should I Do?
Some types of chemotherapy can destroy eggs in your ovaries. This can make it impossible or difficult to get pregnant later. Whether or not chemotherapy makes you infertile depends on the type of drug and your age since your egg supply decreases with age.
"The risk is greater the older you are," Knopman explained. "If you're 39 and you get chemo that's toxic to the ovaries, it's most likely to make you menopausal. But, if you're 29, your ovaries may recover because they have a higher baseline supply."
If your cancer treatment includes surgery in which both ovaries are completely removed, then IVF will likely be needed to help get pregnant.
Radiation to the pelvis can also destroy eggs. It can damage the uterus, too. Surgery to your ovaries or uterus can hurt fertility as well.
Meanwhile, endocrine or hormone therapy may block or suppress key fertility hormones and may prevent a woman from getting pregnant. This infertility may be temporary or permanent, depending on the type and length of treatment.
If you are having a treatment that includes infertility as a possible side effect, your doctor won't be able to tell you for sure whether you will have this side effect. That's why you should discuss your options for fertility preservation before starting treatment.
Dr. Terri Woodard Discusses Options For Preserving Fertility After Cancer
Research shows that women who have fertility preservation prior to breast cancer treatment, in particular, are more than twice as likely to give birth after treatment than those who don't take fertility-preserving measures.
Options For Preserving Your Fertility Before Cancer Treatment
Most women who preserve their fertility before cancer treatment do so by freezing their eggs or embryos.
After you finish your cancer treatment, a doctor who specializes in reproductive medicine can implant one or more embryos in your uterus or the uterus of a surrogate with the hope that it will result in pregnancy. If you freeze eggs only before treatment, a fertility specialist can use sperm and your eggs to create embryos in vitro and transfer them to your uterus.
When freezing eggs or embryos is not an option, doctors may try these less common approaches:
- Ovarian tissue freezing, an experimental approach for girls who haven't yet reached puberty and don't have mature eggs or for women who must begin treatment right away and don't have time to harvest eggs.
- Ovarian suppression to prevent the eggs from maturing so that they cannot be damaged during treatment.
- Ovarian transposition, for women getting radiation to the pelvis, to move the ovaries out of the line of treatment.
In addition to preserving eggs or embryos, positive research has shown that women with early-stage hormone-receptor (HR) positive breast cancer were able to pause endocrine therapy to try to get pregnant and they did not have worse short-term recurrence rates than people who did not stop ET (endocrine therapy). In the study from the Dana-Farber Cancer Institute, most of those people who paused ET were able to conceive and deliver healthy babies.
Of course, your doctor will be able to help you understand your unique circumstances and which path such as pausing endocrine therapy is right for you.
Surrogacy and Gestational Carriers
In some cases after cancer treatment, women may have difficulty giving birth to a child or they may be unable to at all. Having someone else carry their baby may be an option, either through surrogacy or a gestational carrier.
According to the National Cancer Institute, a surrogate pregnancy is "a type of pregnancy in which a woman carries and gives birth to a baby for a person who is not able to have children."
"In a surrogate pregnancy, eggs from the woman who will carry the baby or from an egg donor are fertilized with sperm from a sperm donor to make an embryo," the institute explains.
"The embryo is implanted in the uterus of the surrogate mother, who carries the baby until birth. Surrogate pregnancy may be an option for men or women who want to have children and have had certain anticancer treatments, such as chemotherapy or radiation therapy, that can cause infertility."
As for a gestational carrier, the institute describes this person as a "woman who carries and gives birth to a baby for a person who is not able to have children."
"Eggs from an egg donor are fertilized in the laboratory with sperm from a sperm donor to make an embryo. The embryo is implanted in the uterus of the gestational surrogate, who carries the baby until birth. The gestational surrogate (or carrier) is not genetically related to the baby and is not the biological mother."
If you or someone you know is deciding on whether or not to go the route of surrogacy or gestational carrier, it's important to know that each state has different laws and it may be necessary to speak with an attorney before moving forward.
Questions to Ask Your Doctor
If you're facing cancer treatment and wondering about your fertility preservation options, here are some questions you may consider asking your doctor:
- How do you expect my treatment to affect my fertility?
- Are there specialists I can talk to about my fertility preservation options?
- Is it safe for me to preserve my fertility before treatment?
- What resources are available to help me pay for fertility preservation?
- What mental health resources are available to help me cope with this?
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.

