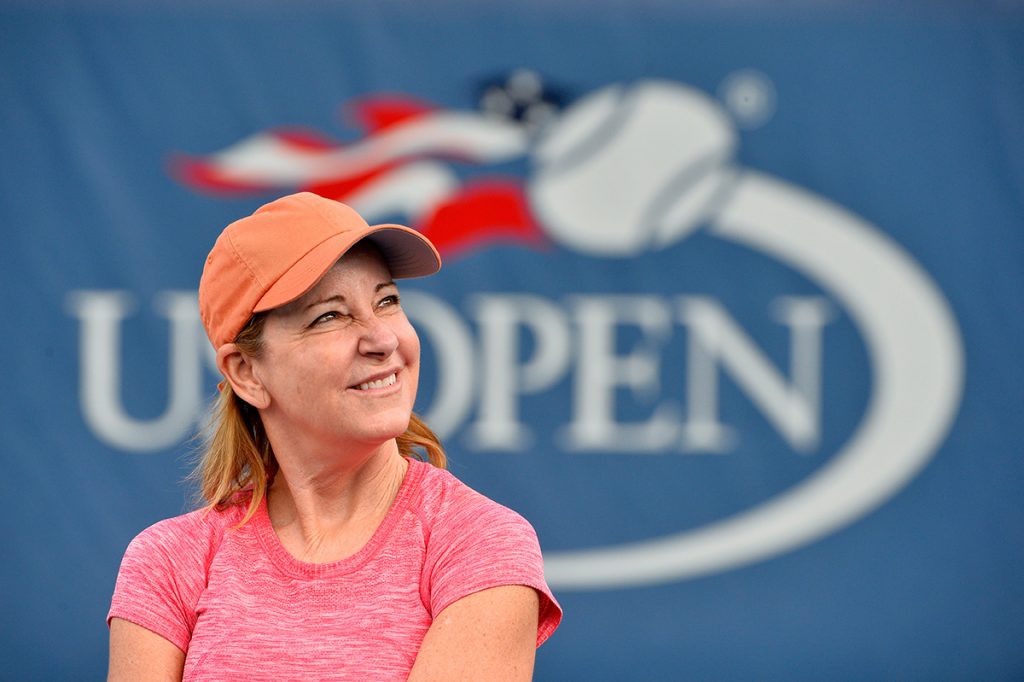
The Impact of Chris Evert Coming Forward
- Tennis legend Chris Evert, 67, recently announced she had been diagnosed with ovarian cancer. Evert’s sister passed from ovarian cancer in February 2020 at the age of 62.
- World-renowned gynecological oncologist Dr. Beth Karlan from UCLA Health says Evert’s treatment path followed the national guidelines for someone of her age range, however, she notes there are various routes a woman can take and these should be discussed with their doctor.
- Dr. Karlan says that Evert’s announcement could eventually become its own “Angelina Jolie Effect.”
Women with a family history of ovarian cancer are at high risk for developing this disease; because of this, doctors encourage that these women get genetic testing. (There are specific genes that raise a woman’s risk for developing ovarian cancer, but more on that in a bit.)
Read MoreIn a recent ESPN article, Evert's diagnosis and what it took to get there is described in vivid detail. Her story, unfortunately, is not an uncommon one, but has a more positive outcome than most ovarian cancer patients because the disease is often caught too late. In Evert's case, she is just stage 1.

While this is obviously an emotional and trying time for Evert and her family, she is sharing her story because, as she says, "any information is powerful."
"Be your own advocate," she tells ESPN. "Know your family's history. Have total awareness of your body, follow your gut and be aware of changes. Don't try to be a crusader and think this will pass."
Here at SurvivorNet, we think world-class medical information should be easily accessible. Evert's story got us thinking about the more than 19,000 women who are expected to be diagnosed with ovarian cancer this year. What are the guidelines for women in Evert's position? How accessible is testing and treatment? We spoke with Dr. Karlan to answer our questions.
"I am not her physician, so I don't know the specifics (of Evert's case)," Dr. Karlan tells SurvivorNet. "But, as a gynecologic oncologist I also direct cancer population genetics for a cancer center I have a lot of insight into what I believe went on."
The Importance of Genetic Testing
Chris Evert's younger sister, Jeanne Evert Dubin, who was also a professional tennis player, died from ovarian cancer in February 2020. She was 62 years old.
When Dubin's cancer was diagnosed, it was in its later stage, and had spread. That is often the case with ovarian cancer, many SurvivorNet experts tell us. Ovarian cancer is almost impossible to diagnose early like in Evert's case because women do not begin to show symptoms until the disease has reached its later stage. There are also no routine screening tests recommended for women who are at an average risk for ovarian cancer.
In that case, how does a woman know if they are at high risk for ovarian cancer? Having a BRCA1 or BRCA2 gene mutation is one way to know. The BRCA1 (BReast CAncer 1) or BRCA2 (BReast CAncer 2) genes help cells repair their DNA damage. Having a change, or mutation, in one of these genes increases a woman's risk of developing ovarian and breast cancer. These gene mutations are commonly passed down in families; if a parent carries a BRCA gene mutation, there is a 50-50 chance you could be carrying it as well.

In Evert's case, the BRCA1 gene is what caught her cancer in its early stage. Here is how:
When her sister was going through cancer treatment, she had tested negative for the BRCA1 gene. Because of this, her family members, including Chris Evert, were not encouraged to seek genetic testing themselves. Dr. Karlan says this is typical: it is not recommended that family members get tested based on a VUS (variant of undetermined significance) result.
"What happens is when you do genetic testing results," Dr. Karlan explains, "it is not always black and white."
However, it was later proven that Dubin did in fact have the pathogenic BRCA1 gene, which increased her chances of developing ovarian cancer. This prompted Chris Evert to "immediately" send her blood in for genetic testing, which revealed she also had the pathogenic variant of the BRCA1 gene. (Gene mutations can either be benign or pathogenic, Dr. Karlan explains.)
It was after conversations with her doctor that Evert decided to have a hysterectomy a surgical procedure to remove the uterus. She had this procedure done first as her sister died of a type of gynecological cancer, but a mastectomy surgery that removes the entire breast was planned for later down the line as BRCA1 can also increase a woman's chances of developing breast cancer.
Dr. Karlan says that while every woman's case is different, Evert followed the appropriate steps to prevent cancer. In fact, women with BRCA1 mutation are recommended to have a prophylactic bilateral salpingo-oophorectomy (PBSO) procedure (the removal of healthy tubes and ovaries in high-risk women to reduce future risk of ovarian cancer) at between the ages of 35 and 40. Chris Evert is 67 years old (she was 65 at the time of discovering she had the mutation), so it was appropriate for her to have a hysterectomy and PBSO upon finding out she has the BRCA1 mutation.
Dr. Karlan explains that women who are still able to have children should be given the option to freeze their eggs for future embryo transfer. This is why it is recommended that younger women only have their tubes and ovaries removed, leaving their uterus in place so they can possibly have children one day. Since Evert is older, she is unable to have more children, so having her uterus removed as well was an appropriate option.
How Accessible is Genetic Testing?
It is recommended that when an individual is found to carry a pathogenic alteration mutation, that their blood relatives be informed and have counseling and testing. So, how accessible is genetic testing?
Dr. Karlan says, "(accessibility) is getting better and better, and it depends on where they (patients) live. … The way it can be done, it is really with saliva."
If you find out that you have a family member who has one of these mutations, if you live in the same city or state, the people that notified your relatives should be able to provide you with the counseling and saliva kit, Dr. Karlan explains. If you live out of state, she recommends checking out the National Society of Genetic Counselors website; you can visit the website to find a counselor and get the referral from there. The saliva tests, she explains, are "just as accurate as it is from the blood."
However, Dr. Karlan notes that commercially available genetic tests, "what I call 'recreational genetics,' the genetic testing that you can do through the ancestry type of kit," like 23andMe, those tests are "not medical grade and should not be done for this." Instead, seek professional medical advice, such as a genetic counselor.
The CA-125 Test: Is it Recommended?
In the ESPN piece detailing Evert's ovarian cancer diagnosis, it was revealed that Evert received regular testing for cancer antigen 125 in her blood.
The CA-125 test can be used to monitor certain cancers during and after treatment, and in some cases can be used to look for early signs of ovarian cancer in women who are at a "very high risk" of developing the disease.
CA-125 is a nonspecific biomarker, but for women with ovarian cancer, it is a good barometer about the activity of the disease.
Ovarian Cancer: The Cancer That Whispers
However, Dr. Karlan's message is clear: this test is not recommended for screening purposes. It is, however, commonly used in ovarian cancer treatment.
"In treatment, we use it to measure the parameter of treatment; in many situations, it has shown to be reliable," Dr. Karlan says. "However, it is not a screening and diagnostic test. If a woman comes in with (cancer) symptoms, CA-125 is not an effective means to find early ovarian cancer."
There are many underlying conditions, such as endometriosis (an often painful condition in which tissue similar to the tissue that normally lines the inside of your uterus grows outside your uterus), that can cause an elevated CA-125. However, that does not mean you have ovarian cancer.
Dr. Karlan adds that scientists still "have not been able to show" that testing for CA-125 can save lives.
The Impact of Chris Evert Coming Forward About Her Cancer
When speaking about the impact of Evert's decision to come forward and speak publicly about her cancer diagnosis, Dr. Karlan spoke of the "Angelina Jolie Effect" something that could happen in Evert's case, as well. (Dr. Karlan was actually Angelina Jolie’s doctor, as well as her mother’s.)

In 2013, Jolie wrote an op-ed in The New York Times coming forward about carrying the BRCA1 gene mutation after her mother died of breast cancer. Three years later, in 2016, a study was published in The BMJ which concluded that there had been a "large spike" in BRCA gene testing following Jolie's piece.
There could be a similar effect since Evert has come forward, Dr. Karlan says. However, it is not something we will know for years to come.
"I think by having someone like Chris Evert I still think of her as Chrissie Evert out there saying, 'Hey, look, you know, I did what I had to do. And boy, I'm glad," Dr. Karlan adds.
"Cancer is a scary word," she says, adding, "Don't be afraid to look into it. Knowledge is power. When you get these results, you're discussing with your physician to decide which course of action is best for you."
Learn more about SurvivorNet's rigorous medical review process.


