Raising Awareness on Melanoma
- College freshman Mari Tisera was 19 years old when she noticed changes to a tiny birthmark on her toe — suddenly she learned her toe needed to be amputated and soon after that, she was facing an advanced stage melanoma diagnosis, yet she continued pursuing her college degree.
- Tragically, Mari then learned that the aggressive skin cancer had spread to her brain. She was just 20 years old when she died from the disease. Mari’s grieving family is now hoping to save others from having to experience their heartbreak. They are bravely sharing her story as an urgent warning to other families and young people about the dangers of skin cancer.
- The most important thing to look out for when it comes to finding melanoma is a new spot on your skin or a spot that is changing in size, shape, or color, SurvivorNet’s medical experts say, and get in to a doctor right away.
Tragically, Mari then learned that the aggressive skin cancer had spread to her brain.
Read More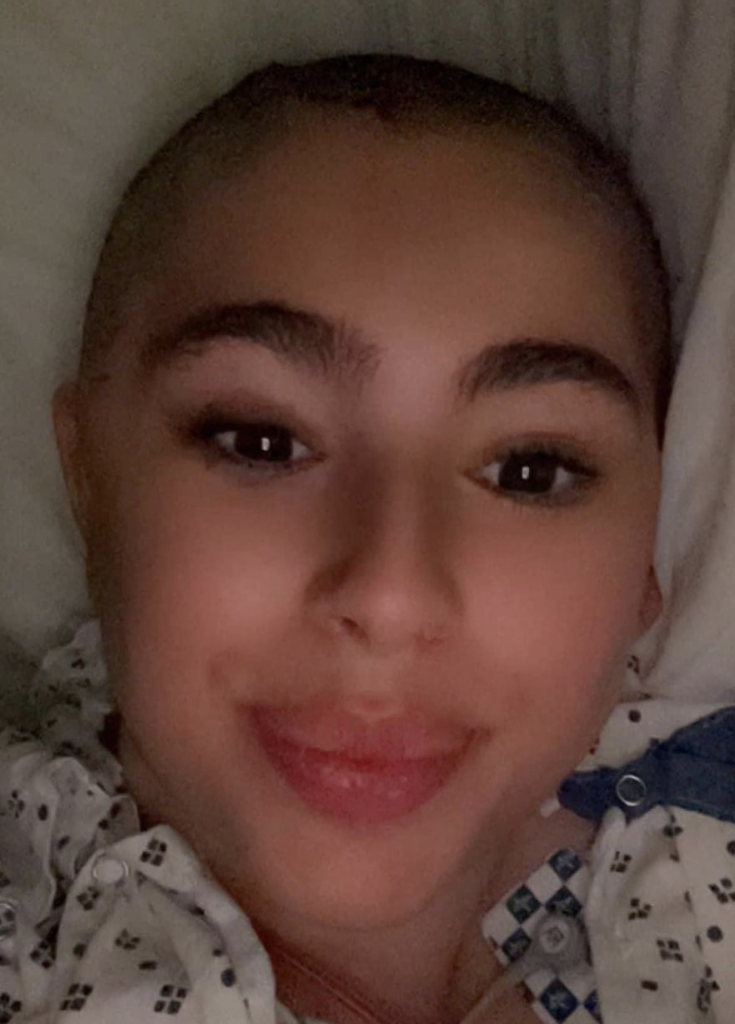
Mari’s mother described how responsible they were overall on health appointments, but getting skin checks at the dermatologist just hadn’t crossed their minds. After all, they had no family history of skin cancer and Mari, she explained, was not fair-skinned, and did not spend a lot of time in the sun. Additionally, like many others, they thought these diagnoses happened to much older people.
“I’m thinking about what we did wrong, but I — you cannot believe how organized we were. We have calendars with all her appointments,” she said, nothing they “never missed any” as she became emotional.

Coping with the immense grief by sharing sweet memories, they understandably would give anything to have had more time with Mari, who was just embarking on her journey into adulthood while away at George Mason University in Northern Virginia.
“Coming in the door every weekend and saying, ‘I’m here! The princess is here!” her mom said. “That is what I miss most.”
In a touching tribute to Mari on George Mason University’s website, McKenna Beauchamp fondly recalled hanging out with her best pal, who was a member of the Zeta Psi sorority.
“She lit up every room. She had no enemies, and her laughter is unlike anything I’ve ever heard.”
View this post on Instagram
The school, for the 32nd time in its history, announced in April they would be honoring Mari with a posthumous degree. Her bachelor of arts in government and international politics was presented to her entire family, including her three big brothers who were in attendance with their wives, on May 10 at EagleBank Arena in Fairfax, Virginia.
“[Mari] never let her cancer define her or hold her back in any way,” McKenna shared, as the school noted how “relentless” she was in advocating for the “rare” posthumous degree. “She worked, she went to school, she would do her homework during her treatments and come to campus to take an exam.”

“She was so strong,” McKenna added, recalling the recent graduation experience and how it has brought a sense of closure for her and Mari’s loved ones. “It’s really a good thing to celebrate.”
In response to the overwhelming support of Mari, the Tiseras expressed “heartfelt gratitude for the immense love, support, and generosity bestowed to Mari and the rest of her family. May she rest in peace.”
Learning More About Melanoma
Melanoma is the most dangerous form of skin cancer. It starts in the same cells that give your skin, hair, and eyes their color. In melanoma, the cells change in a way that allows them to spread to other organs.
Changes to a mole you’ve had for a while or a new growth on your skin could be signs of melanoma, according to SurvivorNet’s experts. You’ll want to watch them and tell your doctor about any changes you notice.
WATCH: How do you perform a skin check using the ABCDEs?
You’re most likely to find melanoma on sun-exposed skin areas like your face, neck, arms, and legs. Surprisingly, you might also find them in other places as well, like:
- The palms of your hands or soles of your feet
- On your eyes or mouth
- Under your nails
SurvivorNet experts recommend avoiding unprotected sun exposure because ultraviolet (UV) radiation can lead to melanoma. Tanning beds pose ultraviolet radiation risks for skin cancer and should be avoided. Many dermatologists recommend using spray tans to reduce the risk of melanoma skin cancer.
What Are the Symptoms of Melanoma?
The most important thing to look out for when it comes to finding melanoma is a new spot on your skin or a spot that is changing in size, shape, or color, SurvivorNet’s medical experts say.
When you check your skin, use the acronym ABCDE as your guide:
- Asymmetrical moles: If you drew a line straight down the center of the mole, would the sides match?
- Borders: Is the mole irregular or jagged?
- Colors: Are there multiple distinct colors in the mole?
- Diameter: Is the mole larger than 6 millimeters (mm), about the size of a pencil head eraser?
- Evolution: Has the mole’s color, shape, or size changed over time?
RELATED: The Genetic Mutation That Drives Many Metastatic Melanomas
If you answered “yes” to any of these questions, our experts say it’s time to see your dermatologist for a skin check.
Melanoma Treatment Options
Melanoma treatment has come a long way. Survival rates have risen dramatically, thanks to a “treatment revolution,” say SurvivorNet’s experts. With breakthrough treatments like targeted therapy and immunotherapy now available, people who are diagnosed today have a much better chance of living a long and healthy life than ever before.
If you’re diagnosed with melanoma, there’s a good chance surgery is going to be the treatment your doctor recommends. In the early stages of the disease, removing the cancer should lead to a cure. The question is typically not whether you’ll get surgery, but which kind you’ll have.
WATCH: Dermatologic Surgeon Dr. Nima Gharavi, On The “Gold Standard Treatment” For Melanoma
For an early-stage melanoma that is close to the skin surface, Mohs surgery might be an option. This technique removes skin cancer, layer by layer, until all the cancer is gone.
In general, stage I melanoma surgery consists of the simple, in-office removal of the cancerous cells by a dermatologist. If the cancer is thicker, your surgeon will remove it through a technique called wide excision surgery.
The removal of stage II and III melanomas are performed by surgeons or surgical oncologists, not dermatologists. You may also have a sentinel lymph node biopsy to see if the melanoma has spread to the first lymph node where it’s most likely to travel. If your cancer has reached this first lymph node, it may have spread to other neighboring lymph nodes, and possibly to other organs. Where the cancer is will dictate your treatment.
After surgery, the removed tissue and lymph nodes will go to a specialist called a pathologist, who will measure the melanoma and find out if it has clear margins. Having clear margins means the cells around the area of tissue that was removed don’t contain any melanoma. When there aren’t any cancer cells left around the removed area, your cancer is less likely to come back.
Once your cancer spreads, treatment gets a little more complicated, but there are still ways to stop it. New treatments have vastly improved the outlook for people with metastatic, or stage IV, melanoma.
Targeted drugs and immunotherapy have been shown to be more effective than chemotherapy. So, with many more choices, there is no standard treatment. Treatment will vary based on your condition and whether there is recurrent disease.
Research has found that immunotherapy drugs such as Keytruda (pembrolizumab) and Opdivo (nivolumab) helped some people live longer. Combining immunotherapy drugs Yervoy (ipilimumab) and Opdivo (nivolumab) has also extended survival. Opdivo (nivolumab) + relatlimab is a new therapy option added to the National Comprehensive Cancer Network guidelines in 2022. The combination of two immunotherapies is called Opdualag.
For those with the BRAF mutation, targeted drugs which shrink or slow the tumor can be a good option. This could include a combination of drugs, such as:
- Zelboraf (vemurafenib) and Cotellic (cobimetinib)
- Braftovi (encorafenib) and Mektovi (binimetinib)
- Tafinlar (dabrafenib) and Mekinist (trametinib)
- Zelboraf (vemurafenib) and Cotellic (cobimetinib) can also be combined with atezolizumab.
“Every patient is different and every situation is different,” says Dr. Anna Pavlick, medical oncologist at Weill Cornell Medicine. She emphasized that “there is no cookie-cutter recipe,” for treating stage IV melanoma.
There Is No “Cookie Cutter Recipe” for Treating Stage Four Melanoma
Dr. Pavlick also notes the importance of personalized care and treatment. “It really is a matter of looking at the tools we have so that we can pick the right tools to give the patient the best outcome.”
So, while there is no one-size-fits-all approach to treating metastatic melanoma, your doctor will work with you to develop a treatment plan that is tailored to your individual situation. Advances in research and technology are making the fight against metastatic melanoma more hopeful than ever.
Questions to Ask Your Doctor
If you are diagnosed with skin cancer, you may have some questions for your doctor. SurvivorNet suggests some of the following to help you on your cancer journey.
- What type of skin cancer do I have?
- What treatment options exist for my type of melanoma?
- Will insurance cover this treatment?
- Would treatment through a clinical trial make sense for me?
- What resources exist to help manage my anxiety because of this diagnosis?
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.

