Why a Growing Number of Younger Women Diagnosed with Breast Cancer
- The former host of “Dancing with the Stars” Samantha Harris, 50, was diagnosed with breast cancer at just 40 years old. A new study published in JAMA Network Open highlights a growing number of women diagnosed with breast cancer under the age of 50.
- The study involved more than 215,000 women from diverse backgrounds between 2000 to 2019. The number of women diagnosed with estrogen receptor-positive (ER+) at stage 1 and stage 4 breast cancer saw an increase.
- Meanwhile, during that same period, the number of women diagnosed with breast cancer estrogen receptor-negative (ER-) and at stages 2 and stage 3 saw a decrease.
- Researchers point to women having children at older ages, increased early detection efforts, and obesity as contributing factors for more young women being diagnosed with breast cancer.
- When a certain type of cancer tests positive for being hormone-receptive, it means that the cancer needs the hormones estrogen and/or progesterone to grow.
- Hormone receptor-positive means the cancer is positive for either the estrogen and/or progesterone receptor. Hormone receptor-negative (HR-) means that your cancer cells don’t have estrogen or progesterone receptors.
“Dancing with the Stars” host Samantha Harris, 50, was just 40 years old when she discovered a lump in her breast after having a “clear” mammogram. She was later diagnosed with breast cancer. Her experience is part of a growing trend researchers at Washington University School of Medicine in St. Louis pinpointed in a new study published in JAMA Network Open.
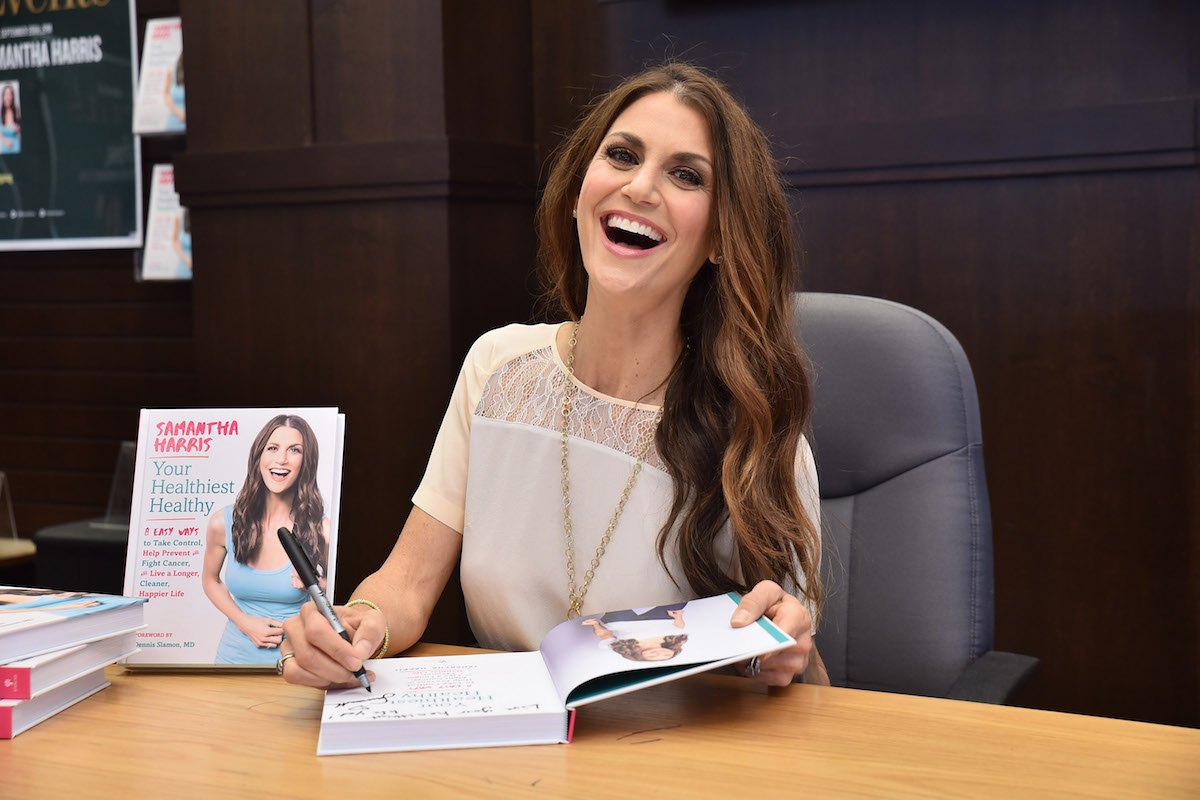
(Getty Images)
Read More
Helping Patients Cope with a Breast Cancer Diagnosis
A Concerning Trend
The research study studied breast cancer incidence rates during a 20-year period from 217,815 women under 50 across multiple racial groups. It aimed to gauge breast cancer rates across racial and ethnic groups, the types of breast cancer, and its hormone receptor status.- Hormone receptor-positive cancers are actually the most common types of breast cancers. When a tumor is “hormone receptor-positive,” it means that a pathologist has run special tests on the cancer to determine that it is positive for either the estrogen and/or progesterone receptor.
- When a certain type of cancer tests positive for being hormone-receptive, it means that the cancer needs the hormones estrogen and/or progesterone to grow.
- Hormone receptor-negative (HR-) means that your cancer cells don’t have estrogen or progesterone receptors. In this case, hormone therapy drugs would not be effective. This type of breast cancer tends to grow more quickly and is more common in women who have not yet gone through menopause. If the cancer returns, it’s more often in the first few years after treatment is completed.
“Non-Hispanic Black women aged 20 to 29 and 30 to 39 years had the highest Age-standardized incidence rates (ASIR) with a rising trend of ASIR and cohort and period effects. However, the incidence rate was highest among non-Hispanic White women aged 40 to 49 years,” researchers added.
Helping Patients Cope with a Breast Cancer Diagnosis
Possible Reasons for the Increase in Breast Cancer Among Younger Women
The researchers pointed to some key areas that may be contributing factors for the increase in breast cancer among women under 50 and possible solutions to reverse the trend.
Black women should consider breast cancer risk assessment screenings at earlier ages. We already know if you have a family history of cancer or have the BRCA gene mutation, which increases your cancer risk, you should consider screening between 30 and 40 years old.
The U.S. Preventive Services Task Force recommends women begin screening for breast cancer at age 40. Women should talk with their doctor to learn about their cancer risk and assess when a good time is to start annual mammograms.
Among Hispanic women, the researchers suggest because they “have children at younger ages, higher maternal parity, and breastfeed for longer periods when compared to non-Hispanic white women, may contribute to them having the lowest incidence rates (of breast cancer)” observed in the study.
Last year, Pew Research said the average age of women giving birth for the first time was 27 years old. That figure has increased from 25 in 2011. Researchers leading the study also noted that the first birth for U.S. women has increased steadily from “1970 to 2017 across all races and ethnicities.” They add that “Older age at first birth has been associated with increased risk of estrogen-positive (ER+) and progestogen-positive (PR+) tumors and reduced risk of estrogen-negative (ER-) and progestogen-negative (PR-) tumors.”
Obesity is another possible contributing factor to the increased breast cancer rate among younger women. The researchers note that “adult body mass index (BMI) was inversely associated with risk of ER-/PR- breast cancer among premenopausal women.”
What Does the Stage of the Cancer Discovered Among Younger Women Tell Us?
Researchers believe the increase in younger women being diagnosed with stage 1 breast cancer can be attributed to better early-detection efforts through public health campaigns. Mammograms, self-exams, and enhanced mammograms such as 3D mammograms are growing in public awareness.
The study also saw an increase in women diagnosed with stage 4 breast cancer. With better early-detection efforts at play, how are some women within this group discovering their cancer at later stages? The answer may rest in current breast cancer screening guidelines.
“Screening for women who are not at an elevated risk, breast cancer is not recommended before age 40, so young women often detect their own breast cancers, which may lead to them not being discovered until they have reached a more advanced stage,” researchers say.
Current breast cancer screening guidelines promote screenings to begin at age 40.
Women who haven’t gone through menopause are encouraged to get a mammogram annually between the ages of 45 and 54. If you have experienced menopause, you can get a mammogram every two years.
The U.S. Preventive Services Task Force recommends women begin screening for breast cancer at age 40. Women should talk with their doctor to learn about their cancer risk and assess when a good time is to start annual mammograms.
“We all agree regular screening mammography saves lives,” Dr. Connie Lehman, a professor at Harvard Medical School, told SurvivorNet.
Women who are at higher risk of getting breast cancer may want to be screened sooner. Suppose you fit into the high-risk category for breast cancer, meaning a close family relative has been diagnosed. People at higher risk may have the BRCA1 or BRCA2 gene mutation or had radiation to the chest area when they were young. In cases like this, people in the high-risk category should begin annual mammograms at 30 years old.
Harris’ Breast Cancer Journey
Harris was diagnosed with breast cancer in March 2014 despite finding nothing during a mammogram.
“It missed the cancer in my right breast,” Harris said on her blog. “Two doctors told me the lump I found 11 days later was ‘nothing.’
“Finally, four months after finding that lump, I went to see a breast cancer specialist (a surgical oncologist), someone whose main job it is to look at breasts all day and specializes in the detection of breast cancer.”

After a follow-up MRI, biopsy, and ultrasound, Harris’ cancer was still not found. But doctors decided to remove some of her breasts for further testing because they could tell “something was not right.”
“We decided to take it out,” she explained. “Thank goodness, because when the pathology from that lumpectomy came back, it was indeed invasive carcinoma, in addition to the less concerning ductal carcinoma in situ.”
She treated her breast cancer with a bilateral mastectomy, also called a double mastectomy, which removes both breasts. After that, she underwent breast reconstructive surgery.
During reconstruction, plastic surgeons can reconstruct your breasts with implants or with your tissue taken from some other place on your body, such as your back, your abdomen, or your inner thigh.
Harris’ cancer did spread to one lymph node, but doctors decided she didn’t need chemotherapy or radiation.
The mother of two has since been declared “cancer-free” with close monitoring “for the rest of what doctors tell [her] is sure to be a long, healthy life.”
Learn more about SurvivorNet's rigorous medical review process.

