Breast Cancer and Fertility
- Actress Shannen Doherty, 52, revealed she received several rounds of in vitro fertilization (IVF) to boost her chances of having a child with her ex-husband. She revealed she believed her IVF treatments were linked to her eventual breast cancer diagnosis.
- Dr. Jaime Knopman, Director of Fertility Preservation at CCRM, New York, says the increased breast cancer risk likely has more to do with the population of women who get fertility treatment and their health characteristics rather than the actual drugs they are being given to stimulate their fertility.
- Various cancer treatments, including chemotherapy and radiation, can affect both men’s and women’s fertility. IVF is among several options cancer patients can turn to if they have hopes of parenthood.
- Before undergoing cancer treatment, patients must speak to their doctors about fertility preservation if they wish to have a family in the future.
- Egg, sperm, and embryo freezing are common approaches to fertility preservation, but other options exist.
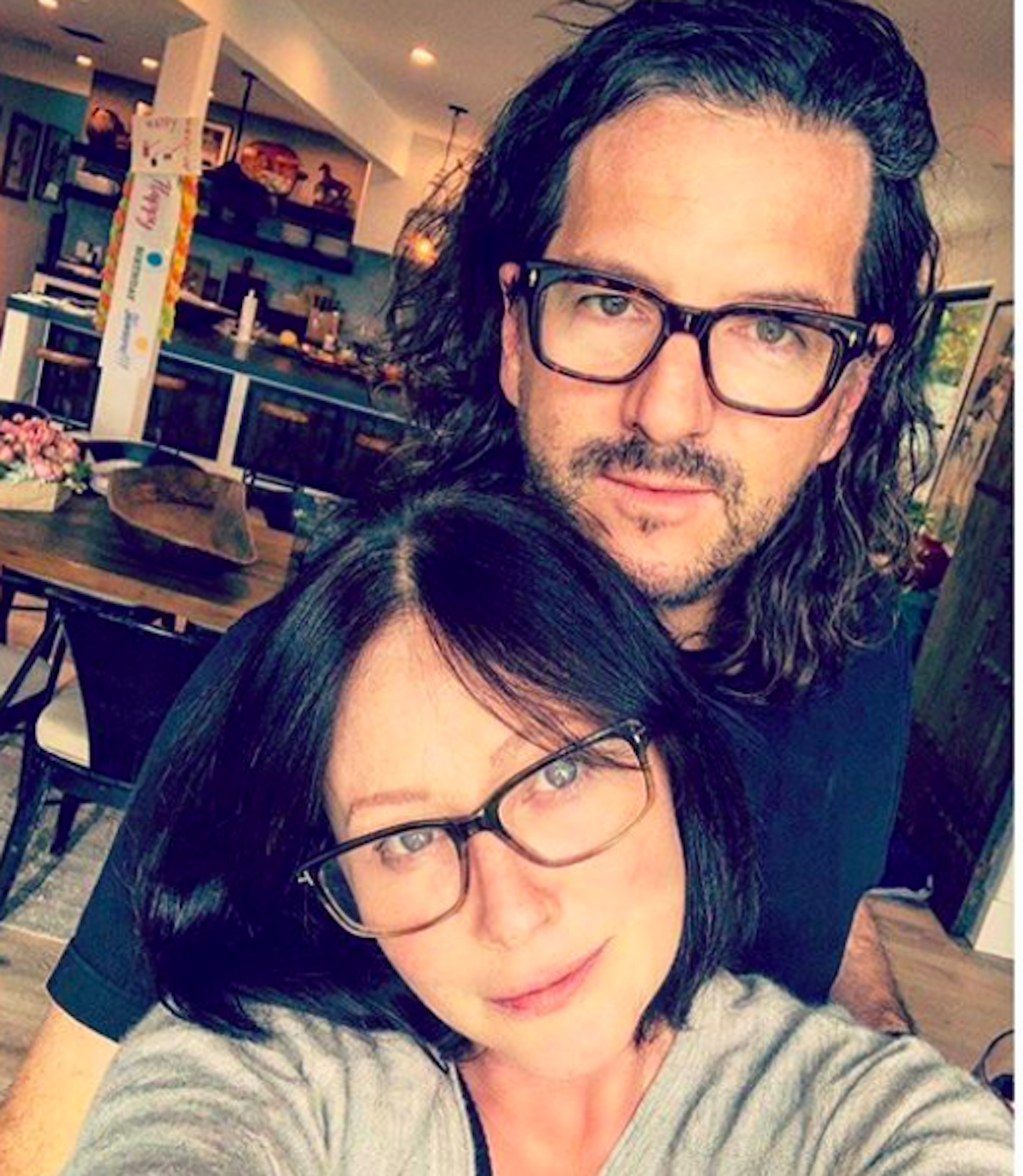
Brave actress Shannen Doherty, 52, is shedding light on her desire to be a mom. She also revealed what she believes contributed to her eventual breast cancer diagnosis. Doherty said she began in vitro fertilization (IVF) treatments to boost her chances of having a child with her ex-husband Kurt Iswarienko several years ago.
During a recent episode of Doherty’s podcast, she claimed because she received “a bunch of rounds of (IVF),” the treatment contributed to her getting breast cancer.
Read More
While Doherty noted her beliefs were based on “anecdotal evidence.” However, a previous study suggested that women who undergo IVF are more likely to be diagnosed with breast cancer, with an added caveat other factors must be considered.
The 2019 study, presented at the European Society of Human Reproduction and Embryology conference in Vienna, involved 59,000 women who had fertility treatment and 567,000 females of equal age who had not. Over the 21-year period that the study spanned, less than 1 percent of the total 626,000 women were diagnosed with breast cancer, with those who had utilized IVF getting the disease at a higher rate.
“If you sort of have a cell that’s a little wonky and that’s sitting on the edge of maybe turning, spreading cancer…that all the hormones that you’re pumping into your body from IVF are only going to up that chance. That was at least my thinking,” Doherty explained.
The Irish Independent also reported on the 2019 study and added that “Scientists believe estrogen given to women to stimulate the ovaries into producing more eggs in preparation for IVF may explain the cancer link.”
Dr. Jaime Knopman, Director of Fertility Preservation at CCRM, New York, explained to SurvivorNet that the increased breast cancer risk likely has more to do with the population of women who get fertility treatment and their health characteristics rather than the actual drugs they are being given to stimulate their fertility. Part of the reason involves the amount of time women spend producing eggs.
“The menstrual cycle of hormones does place someone at risk for breast cancer,” says Dr. Knopman. “When you are pregnant, you are ten months out of the period game– then breastfeeding.” As a result, pregnancies can help protect against cancer by reducing the amount of period cycles women go through during their childbearing years.
Dr. Knopman adds another way that the data suggesting IVF is linked to cancer gets skewed.
“People who do in vitro fertilization also have a better follow-up because when people come in for in vitro fertilization, we make them get a mammogram. That may put diagnoses at a falsely higher level.”
Doherty was first diagnosed with breast cancer in 2015, and her belief that IVF may contribute to cancer risk led her to decline using tamoxifen after she reached remission in 2017.
Tamoxifen is a selective estrogen receptor modulator, which means it works to prevent estrogen from helping cancer cells to grow. It is also used to prevent breast cancer among women who are at high risk for breast cancer because of family history. One notable side effect of tamoxifen is the mimicking of menopause, which is something Doherty claimed to have already been experiencing.
“When I got the ‘You’re all clear’ remission after chemo and all of that, I knew I wasn’t doing IVF anymore because I was already in menopause.
“My decision was, at the time, based on sort of the facts that I knew, that I had investigated, and you, in fact, did keep on encouraging me to take the Tamoxifen, and I was like, ‘Absolutely not,” Doherty said to Dr. Lawrence Piro, the President and CEO of the Angeles Clinic and Research Center at Cedars-Sinai during the podcast interview.
Doherty’s doctor said that she was “desperate” to conceive a child with her ex-husband.
However, Doherty and Iswarienko divorced last year as she continued stage 4 cancer treatment.
“I have looked at adopting and all sorts of different options. I think I struggled a lot with my cancer diagnosis and how fair it is. I’m in treatment, and I’m going to see if that treatment works. See what’s coming down the pipeline, what clinical trials, and if I feel like I can give a long enough time to a child, then I’ll definitely do it,” Doherty said of her continued desires to become a mom.
Helping Patients With Fertility Resources
IVF as an Option for Cancer Patients
Cancer treatments like chemotherapy can damage sperm in men, and hormone therapy can decrease sperm production, according to the National Cancer Institute. Radiation treatment can also lower sperm count and testosterone levels, impacting fertility.
These possible side effects of cancer treatment should be discussed with your doctor before starting treatment. For male cancer patients, men may have the option to store their sperm in a sperm bank before treatment to preserve their fertility.
This sperm can then be used later as part of in vitro fertilization (IVF), a procedure in which a woman’s egg is fertilized with sperm in a lab. The embryo is then transferred to a woman’s uterus to develop.
Cancer Treatment’s Impact on Fertility in Women
Just as cancer treatment can impact men’s fertility, women may also be affected. Some types of chemotherapy can destroy eggs in your ovaries. This can make it impossible or difficult to get pregnant later. Whether or not chemotherapy makes you infertile depends on the drug type and age since your egg supply decreases with age.
“The risk is greater the older you are,” reproductive endocrinologist Dr. Jaime Knopman told SurvivorNet.
“If you’re 39 and you get chemo that’s toxic to the ovaries, it’s most likely to make you menopausal. But, if you’re 29, your ovaries may recover because they have a higher baseline supply,” Dr. Knopman continued.
Radiation to the pelvis can also destroy eggs. It can damage the uterus, too. Surgery to your ovaries or uterus can hurt fertility as well.
Meanwhile, endocrine or hormone therapy may block or suppress essential fertility hormones and may prevent a woman from getting pregnant. This infertility may be temporary or permanent, depending on the type and length of treatment.
If you have a treatment that includes infertility as a possible side effect, your doctor won’t be able to tell you whether you will have this side effect. That’s why you should discuss your options for fertility preservation before starting treatment.
Research shows that women who have fertility preserved before breast cancer treatment are more than twice as likely to give birth after treatment than those who don’t take fertility-preserving measures.
Most women preserve their fertility before cancer treatment by freezing their eggs or embryos.
After you finish your cancer treatment, a doctor specializing in reproductive medicine can implant one or more embryos in your uterus or the uterus of a surrogate with the hope that it will result in pregnancy.
If you freeze eggs only before treatment, a fertility specialist can use sperm and eggs to create embryos in vitro and transfer them to your uterus.
When freezing eggs or embryos is not an option, doctors may try these approaches:
- Ovarian tissue freezing is an experimental approach for girls who haven’t yet reached puberty and don’t have mature eggs or for women who must begin treatment immediately and don’t have time to harvest eggs.
- Ovarian suppression prevents the eggs from maturing so they cannot be damaged during treatment.
- For women getting radiation to the pelvis, Ovarian transposition moves the ovaries out of the line of treatment.
In addition to preserving eggs or embryos, positive research has shown that women with early-stage hormone-receptor (HR) positive breast cancer were able to safely pause endocrine therapy (ET) to try to get pregnant, and they did not have worse short-term recurrence rates than people who did not stop endocrine therapy.

Doherty’s Cancer Journey
Shannen Doherty’s initial breast cancer diagnosis arrived in 2015 after she discovered a lump in her breast. For treatment, she had hormone therapy, a single mastectomy (the removal of all breast tissue from one breast), chemotherapy, and radiation.
In 2017, she achieved remission status, but the disease returned two years later in 2019. This time around, her breast cancer was metastatic, or stage 4.
Having metastatic breast cancer means the cancer has spread, or metastasized, beyond the breasts to other parts of the body. It often spreads to the bones, liver, and lungs but can also spread to places like the brain.
While treating advanced breast cancer, the goal of treatment is to keep you as stable as possible, slow the tumor growth, and improve your quality of life.
WATCH: Aggressive breast cancer in younger women.
As cancer treatments improve year over year, so does the number of people battling this form of cancer that spreads to the brain, says Dr. Michael Lim, who is the Chair of the Department of Neurosurgery and a board-certified neurosurgeon specializing in brain tumors at Stanford Medicine.
According to Dr. Kimberly Hoang, a board-certified neurosurgeon at Emory University School of Medicine, a craniotomy procedure like Doherty underwent earlier this year is “a procedure to cut out a tumor” on the brain that may be particularly useful “if the tumor is causing symptoms or if it’s large.”
Since undergoing brain surgery, Doherty has focused on enjoying precious time with loved ones as she continues battling stage 4 cancer.
Doherty’s cancer then spread, or metastasized, to her brain. As a result, she’s undergone both radiation and surgery in the form of a craniotomy to improve her prognosis.
Questions for Your Doctor
If you’re wondering how your cancer treatment may affect your fertility and what options are available to you, consider asking your doctor these questions, according to the National Cancer Institute:
- Could my treatment lead to infertility?
- Are there other recommended cancer treatments that might not cause fertility problems?
- Which fertility preservation options would you advise for me?
- What fertility preservation options are available at this hospital? At a fertility clinic?
- Would you recommend a fertility specialist (such as a reproductive endocrinologist) I could talk with to learn more?
- What are the chances that my fertility will return after treatment?
Learn more about SurvivorNet's rigorous medical review process.

