Understanding Prostate Cancer Surgery and Navigating Its Side Effects
- Veteran journalist Rob Vaughn announced he’s undergoing prostate cancer surgery and will step away from the anchor desk to focus on treatment.
- A prostatectomy is a surgical procedure for prostate cancer. It’s an option for men with any risk group of prostate cancer that hasn’t spread outside of the prostate gland.
- During this procedure, the surgeon removes the entire prostate, along with some tissue around it, including the seminal vesicles that release fluid into the semen. Side effects may follow this procedure, which may include erectile dysfunction and urinary incontinence.
- The nerve-sparing surgery option can reduce the risk of side effects like sexual dysfunction, though it may not be suitable for everyone. Nerve-sparing surgery involves removing cancer without harming the nerves, but if the cancer is near the nerves, it may need removal.
- Surgery may not be needed for all men diagnosed with prostate cancer. In some cases, active surveillance is a preferred treatment option for older men or those with a low risk of the disease spreading. It helps people avoid unnecessary treatment and side effects.
Prostate cancer surgery is one treatment avenue for men grappling with this disease. However, surgery may bring forth lingering side effects, such as erectile dysfunction. Thankfully, there are avenues available to alleviate some of these challenges.
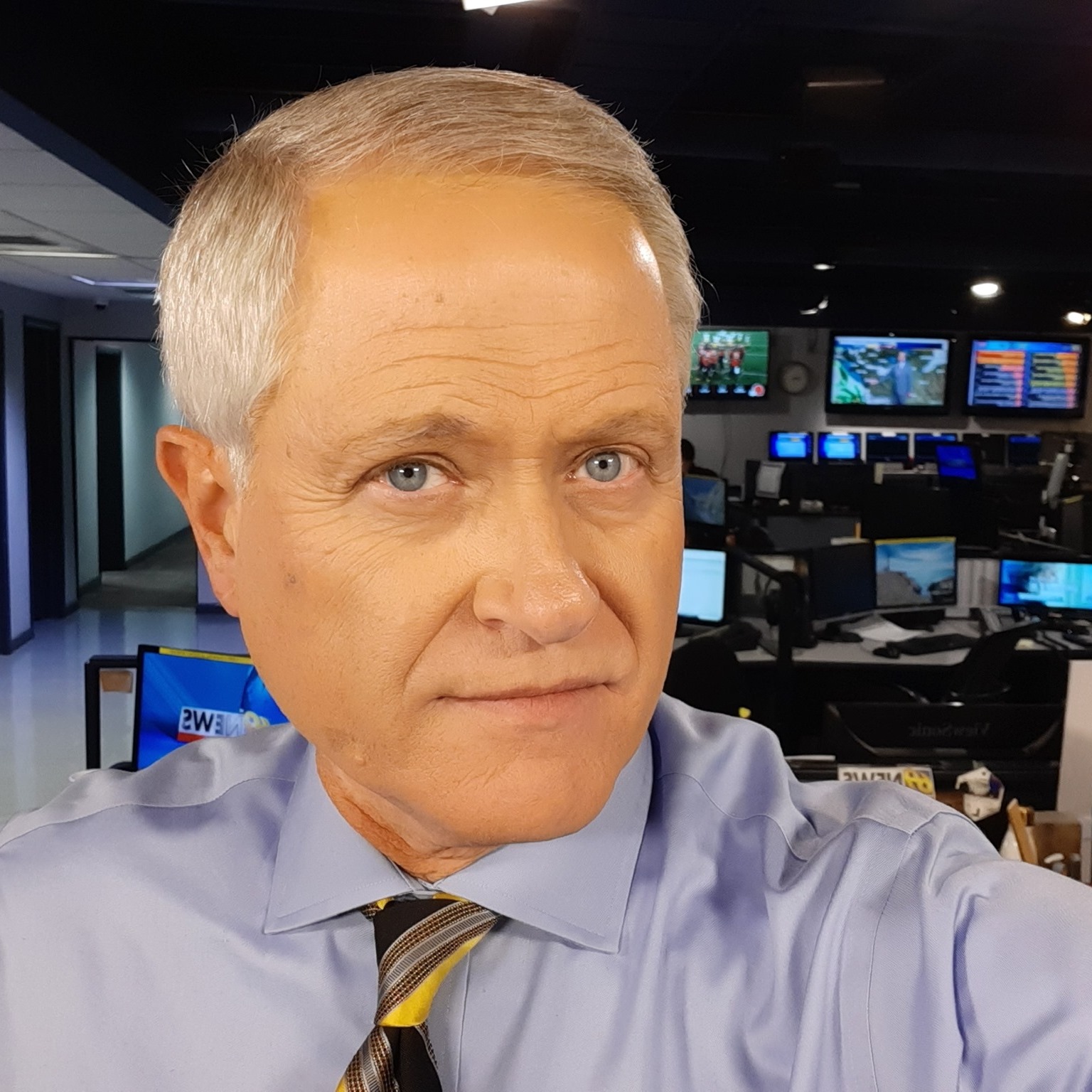
“All our love and prayers for a speedy recovery, RV…big hugs,” Vaughn’s fellow news anchor Eve Russo wrote in a Facebook comment.
“Best of luck. Three months after my 2023 prostate cancer, I was riding my bicycle all over the local trails. Last month, I was pronounced cancer-free,” Facebook user Mike Hnatow commented.
Amid the flood of well-wishes, Vaughn thanked everyone for their support.
“Thank you everyone for the wishes and thoughts and prayers. I’m saying this here because I don’t know if I’ll be able to put Likes and other reactions on all the comments! Too many. Thank you,” Vaughn said.
Helping Patients Understand Prostate Cancer Treatment Options
Surgery Options for Prostate Cancer
Prostate cancer treatment depends on the results of a prostate exam, your PSA numbers, and your Gleason Score, which helps determine how aggressive the cancer is.
Your doctor will determine your risk level, which ranges from low to intermediate to high. Men with low risk and very low risk may bypass surgery. Meanwhile, men at higher risk may receive more intense treatment.
WATCH: Dr. David Wise, NYU Langone medical oncologist, explains how Gleason’s score affects treatment and prognosis.
Surgery is an option for men with any risk group of prostate cancer that hasn’t spread outside of the prostate gland. The surgery procedure is called a radical prostatectomy. During this procedure, the surgeon removes the entire prostate, along with some tissue around it, including the seminal vesicles that release fluid into the semen. Your doctor can perform this through a traditional open procedure called laparoscopic surgery with one large or several small incisions.
“It’s typically done through a robotic technique today, at least in the United States, but a lot of patients are still getting open surgery,” Dr. Stephen Freedland, a urologist at Cedars-Sinai Medical Center, explained to SurvivorNet.
“Depending on the surgeon, it may be two, three, four, five hours — somewhere in that range, usually spend one night in the hospital. You wake up from the surgery with a catheter in your bladder. Once you’re home, it’s really just recovering, gaining your strength back,” Dr. Freedland continued.
WATCH: How do you choose the right surgeon, particularly for robotic surgery?
Other common treatment options for men with prostate cancer include:
Radiation therapy.
You’ll usually get this treatment five days a week for several weeks. Newer techniques include stereotactic body radiotherapy (SBRT), which aims for more focused radiation beams at the tumor to spare surrounding healthy tissues and may allow treatment in a shorter time.
Brachytherapy implants small seeds containing radiation directly into your prostate. This type of radiation works best in men with smaller prostates.
If your prostate is very large, your doctor might give you hormone therapy first to shrink it.
Combination radiation therapy with hormonal therapy.
Androgens are male hormones that fuel the growth of prostate cancer. Androgen deprivation therapy (ADT), also known as hormone therapy, reduces levels of these hormones your body makes to slow the cancer’s growth.
“Usually, for men with tumors that spread, hormonal therapy is usually the first line that we do, and more importantly, it’s the backbone upon which we build,” Dr. Freedland explained to SurvivorNet.
Surgery followed by radiation.
Radiation therapy can be used after surgery to get rid of any cancer cells that were left behind. Getting radiation along with surgery is called adjuvant therapy.
Sometimes, men who have surgery will need radiation therapy after surgery if the surgeon cannot remove all of the prostate, your PSA does not become undetectable, or you have a high-risk genetic profile if the tissue is sent for testing.
Men with high-risk and very high-risk prostate cancer are more likely to require radiation after surgery than men with lower-risk disease.
The Side-Effects of Prostate Cancer Surgery
Prostate cancer warriors need to ask their doctor questions about the side effects of surgery.
Some of the known side effects of prostate cancer surgery include erectile dysfunction (difficulty getting or keeping an erection) and urinary incontinence (leaking urine by accident).
Treatments for prostate cancer, especially surgery, can damage nerves and blood vessels essential for erectile function, leading to ED. The risk for these side effects depends on the type of surgical approach and factors specific to your cancer.
WATCH: Sexual Function Recovery After Prostate Cancer Surgery
“Erectile function is so sensitive when we’re dealing with prostate cancer because of the fact that the nerves that are critical for this function wrap around the prostate; they’re just so intimately connected to the prostate that they can be damaged from a surgical removal of the prostate or through radiation treatment,” Dr. Isla Garraway, a staff urologist in the Veterans Administration (VA) Greater Los Angeles Healthcare System, tells SurvivorNet.
Dr. Freedland says that most people regain normal function in these areas over time.
Opting for nerve-sparing surgery can reduce this risk, though it may not suit everyone. Nerve-sparing surgery involves removing cancer without harming the nerves, but if the cancer is near the nerves, it may need removal.
Within a year of nerve-sparing prostatectomy, 40% to 50% of men are back to their pre-cancer sexual function.
For men experiencing erectile dysfunction, they should know there are plenty of solutions.
Oral medications — usually a pill — work for mild to moderate ED by enhancing blood flow to the penis to bring on an erection.
There are medications currently on the market that can aid in sustaining erections, such as Viagra, Cialis, and Levitra. There are also treatments such as penile injections and vacuum erection devices (VED), as well as the option of a penile prosthesis. Vacuum erection devices use vacuum pressure to draw blood into the penis, inducing an erection.
Dr. Freedland says there are two main prosthetic options: an inflatable prosthesis placed in the scrotum or a bendable plastic prosthesis.
According to Dr. Freedland, most men who choose this route report being pleased with the outcome.
Doctors often recommend sexual counseling after prostate cancer treatment to help improve sexual function. This approach actively addresses the psychological, emotional, and relationship impacts on sexual health.
In counseling, individuals and couples can discuss concerns, explore sexual aids and techniques, and find ways to maintain intimacy.
Surgery Isn’t Always the First Option; Some Choose ‘Active Surveillance’
It’s common for prostate cancer to grow very slowly. Some men, especially those who are older and those who have a low risk of the cancer spreading, may not need aggressive treatment, making active surveillance a viable option.
WATCH: People With Low-Risk Prostate Cancer Can Rely on Monitoring the Disease
Active surveillance means the doctor watches the cancer carefully for changes, with a PSA blood test every six months and a digital rectal exam about once a year. You may also get prostate biopsies and imaging tests every one to three years.
SurvivorNet experts stress active surveillance is not “watchful waiting.” Active surveillance is a treatment, and as the name implies, it is active. This path requires coordination between the patient and their healthcare team.
“[It’s] not just kind of check in once a year—hey, how are you doing—but actively have a physician check a PSA and do a rectal examination,” Dr. Edwin Posadas, director of the Translational Oncology Program at Cedars-Sinai Medical Center, told SurvivorNet.
“We can actually see some of the metabolic information within the cells through our next-generation imaging and find high-risk areas that are or are not changing in a patient to let us know, yeah, that cancer’s still sleeping. Let’s not bother– let’s not put that young man through the risk of losing his sexual quality of life or his urinary quality of life,” Dr. Posadas added.
Half of men who choose this approach will avoid unnecessary treatment and potential side effects.
But the other half of men do end up having treatment, whether as a personal decision to remove the cancer or to treat the disease as it progresses. Your doctor will determine if this is necessary based on the results of your ongoing tests.
Learn more about SurvivorNet's rigorous medical review process.

