Making Progress in Glioblastoma Research
- It is known that the herpes virus human cytomegalovirus (HCMV) is linked to glioblastoma cases, but as far as whether or not it specifically causes the aggressive brain cancer has yet to be determined.
- However, for the first time, a study published in March out of France says “mounting evidence is identifying human cytomegalovirus (HCMV) as a potential oncogenic virus.” Oncogenic meaning potentially causing cancer.
- Glioblastoma, or GBM, is considered a central nervous system (CNS) tumor. According to the National Cancer Institute, the average survival rate is 15 months with treatment and less than six if left untreated.
- Glioblastomas are tricky to treat and manage because their cells are heterogeneous, meaning that each one must be individually targeted to slow tumor growth. Surgery cannot remove all the cancer because the tumor burrows into the brain, so the tumor starts to grow again immediately after surgery.
There is reportedly a link, but not yet confirmed as an official cause. However, the HCMV virus is found in most glioblastoma cases, according to a study in a respected medical journal called Cancer Gene Therapy. The discussion has reportedly been going on in the medical community for years.
Read MoreAccording to the study authors, these latest results “fit with an HCMV-incuded glioblastoma model of oncogenesis in vivo, which will open the door to new therapeutic approaches and assess the anti-HCMV treatment as well as immunotherapy in fighting [GBM].
It is important to note that there are over 100 herpes viruses and one of the types that affects humans, Epstein-Barr Virus (EVB), increases a person’s chance of getting nasopharyngeal cancer (in the back of the nose) and types of fast-growing lymphomas, according to American Cancer Society (ACS). ACS says EVB is also potentially linked to Hodgkin lymphoma and some cases of stomach cancer.
Understanding Glioblastoma Tumors
Glioblastoma is considered a central nervous system (CNS) tumor.
According to the National Cancer Institute, the average survival rate is 15 months with treatment and less than six if left untreated. While there is a five-year survival rate of averaging 6 percent, those individuals will never be cancer-free and must continue receiving radiation and chemotherapy for the rest of their lives.
Glioblastomas are tricky to treat and manage because their cells are heterogeneous, meaning that each one must be individually targeted to slow tumor growth. Surgery cannot remove all the cancer because the tumor burrows into the brain, so the tumor starts to grow again immediately after surgery.
In addition to the latest hCMV link, glioblastoma risk factors can include:
- Prior radiation exposure
- Gender: men are more likely to get glioblastoma than women
- Age: people 50 years or older
- Certain genetic syndromes, including neurofibromatosis, tuberous sclerosis, von Hippel-Lindau disease
Symptoms for glioblastoma can vary depending on the area of the brain where the tumor begins and spreads and its growth rate, according to MD Anderson Cancer Center. But common symptoms of glioblastoma can include:
- Headaches
- Seizures
- Changes in mental function, mood, or personality
- Changes in speech
- Sensory changes in hearing, smell, and sight
- Loss of balance
- Changes in your pulse and breathing rate
- Current Options to Treat Glioblastoma
Although glioblastomas are difficult to treat, the Food and Drug Administration’s (FDA) approval of the drug temozolomide (Temodar) was a massive breakthrough in helping patients with this aggressive disease. Temozolomide is a chemotherapy drug patients can take after surgery and radiation therapy.
Dr. Daniel Wahl, professor of radiation and oncology at the University of Michigan, previously explained to SurvivorNet that Temozolomide is an oral drug that works by “slowing down tumor growth.”
“Patients with GBM have effective treatment options; there are four of them: surgery, radiation, chemotherapy, and tumor targeting fields. These are electric fields that we can use to treat these cancers,” Dr. Wahl said.
Watch SurvivorNetTV film ‘Breakthrough,’ the powerful and inspiring story of immunologist and Nobel Prize Winner Dr. Jim Allison
Other FDA-approved drugs for treating glioblastoma include lomustine (Gleostine), intravenous carmustine (Bicnu), carmustine wafer implants, and Avastin (bevacizumab). Avastin is a targeted drug therapy that blocks glioblastoma cells from requesting new blood vessels that feed and allow the tumor to grow.
“Outcomes for these patients are still suboptimal,” Dr. Wahl continued. “What I tell my patients is that we have these effective treatments, but what they do is they delay the time to when this tumor comes back. Only in exceptional circumstances would we ever talk about getting rid of one of these cancers a few.”
Sen. Edward Kennedy’s Glioblastoma
Sen. Kennedy shared his brain cancer diagnosis with the public on May 20, 2008, three days after suffering a seizure.
At the time, there were few who knew as much about cancer and had the power to convene the nation’s top oncologists, something Kennedy did three days later when doctors from the top cancer care centers and medical schools in the country flew to Boston or participated by phone in what may still be the most prestigious tumor board assembled in this country.
Opinion at the time was mixed, with some favoring chemotherapy and radiation, while others felt a more aggressive approach was required that would involve surgery to remove the tumor.

Two weeks after that meeting, Kennedy flew from Massachusetts to North Carolina, where he underwent a four-hour operation at Duke University Medical Center.
Dr. Allan Friedman performed that operation, noting it was “successful” and that the politician was awake during the resection, and should therefore experience no permanent neurological effects from the surgery.
Kennedy then returned to his home state where he began receiving radiation and chemotherapy treatment at Massachusetts General Hospital under the supervision of Dr. Larry Horowitz.
Fighting glioblastoma with electrical fields
When he was diagnosed in May 2008, the best prognosis was that with the aggressive surgery, radiation, and chemotherapy Kennedy had a life expectancy of three to 15 months.
Kennedy rejected that at the time. He passed away on August 25, 2009, 15 months and eight days after first being diagnosed with brain cancer.
The course of treatment Kennedy received, first at Duke and then Mass General, is similar to the treatment that is currently used on patients diagnosed with glioblastoma.
Senator McCain’s Glioblastoma
On July 14, 2017, McCain underwent surgery at the Mayo Clinic to remove a blood clot above his eye. During the course of that procedure, doctors noticed a growth that was later identified as a glioblastoma.
What followed next was almost a mirror image of Sen. Kennedy’s treatment. Sen. McCain, who was 80 at the time, had surgery to remove to tumor. He underwent chemotherapy and radiation.
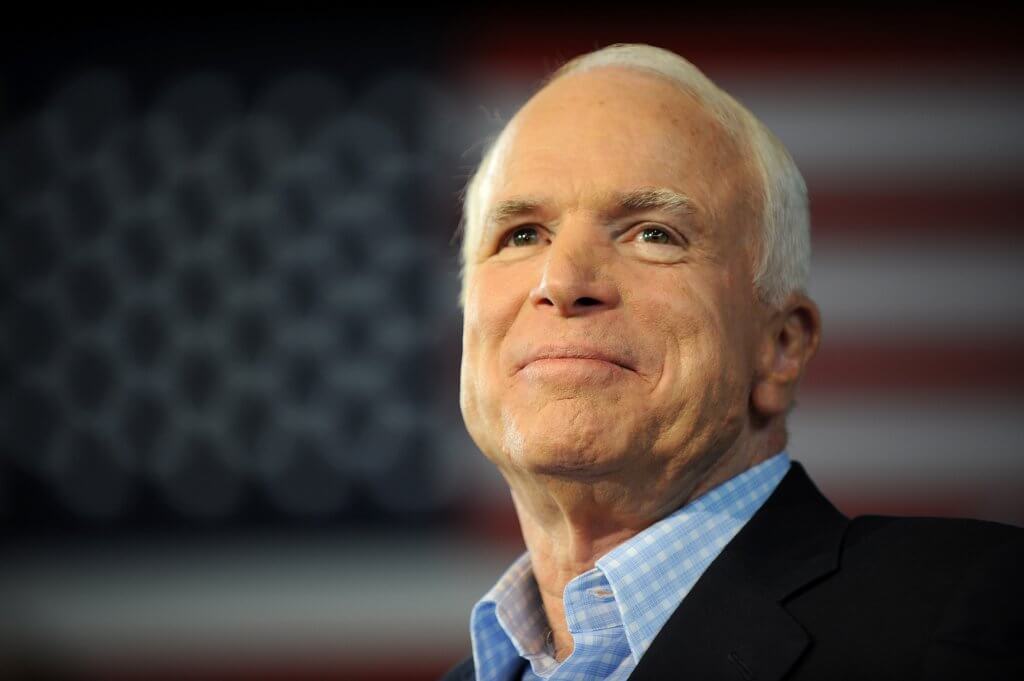
There were also a number of differences between the two men at the time of their diagnosis.
A melanoma survivor, McCain had a number of underlying conditions. He had also developed diverticulitis that required surgery one month after he was diagnosed with his tumor.
Brave until the end, he died on August 25, 2018, 13 months after his diagnosis.
Clinical Trials for Glioblastoma Treatment Show Promise
Researchers have made progress using CAR T-cell Therapy, a cancer treatment that re-engineers the immune system to target cancer. More specifically, researchers used a CAR T-cell therapy variant called CAR-TEAM. It’s designed to be “directly injected into the patient’s brain” by targeting a protein often found in glioblastomas called EGFR.
Although the clinical trial phase for this treatment is far from complete, it presents an opportunity for further exploration of treating glioblastoma.
The results of the clinical trial showed significant tumor regression among patients.
“These results are exciting, but they are also just the beginning—they tell us that we are on the right track in pursuing a therapy that can potentially change the outlook for this intractable disease. We haven’t cured patients yet, but that is our audacious goal,” Dr. Marcela Maus, director of the Cellular Immunotherapy Program at the Mass General Cancer Center, said.
As the clinical trial continues, the team of researchers hopes to find ways to prolong the CAR-TEAM cell treatment’s effectiveness, as two of the three patients experienced a relapse after some time.
Learn more about SurvivorNet's rigorous medical review process.

