Continued Hope for Endometrial Cancer Patients as More Treatments Emerge
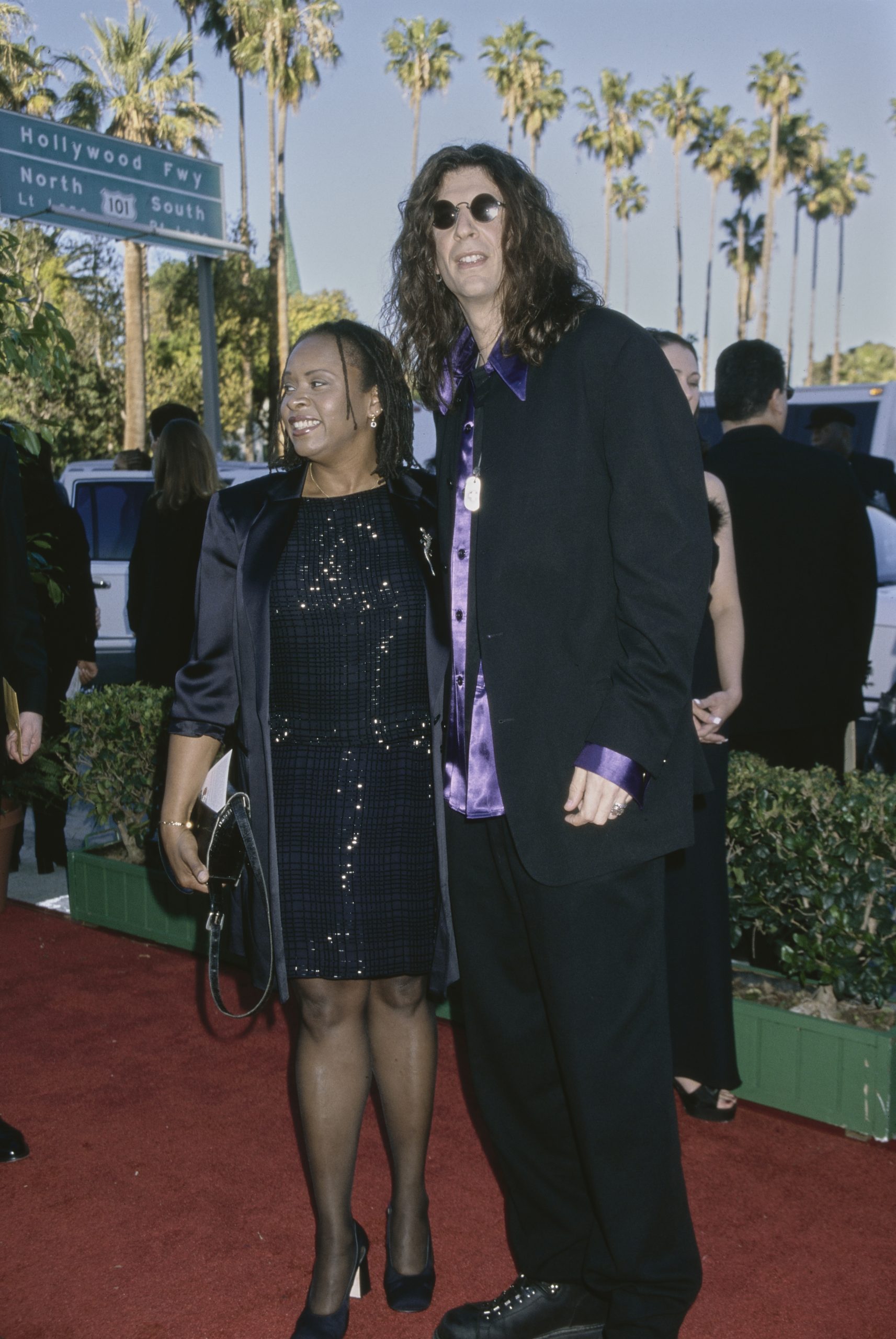
- Popular “Howard Stern Show” sidekick Robin Quivers, 71, was diagnosed with stage 3 endometrial cancer in 2012. Trouble urinating kickstarted doctors’ quest to discover a grapefruit-sized mass on organs in her pelvic area. She underwent a hysterectomy, chemotherapy, and radiation and continues immunotherapy for treatment.
- Endometrial cancer patients have had more treatment options in recent years, as new combination therapies are allowing them to live longer, healthier lives. Immunotherapy and chemotherapy have been shown to help slow disease progression compared to chemo alone.
- Immunotherapy drugs like Durvalumab (brand name Infinzi) work by re-engineering the body’s immune system to fight cancer.
- Olaparib (brand name Lynparza) is a PARP inhibitor, a type of drug that helps treat some cancers by blocking an enzyme called PARP that helps repair damaged DNA in cells. Olaparib destroys cancer cells, especially cells that already have trouble repairing their DNA. Sometimes, it’s used as an add-on to durvalumab to improve progression-free survival (how long a patient lives without their disease worsening).
- Patients with advanced or recurrent endometrial cancer who have a specific set of genetic mutations called mismatch repair deficiency (dMMR) or microsatellite instability-high (MSI-H) can now be prescribed the immune checkpoint inhibitor, dostarlimab-gxly (brand name Jemperli) and chemotherapy.
- Endometrial cancer begins when cancerous cells form in the tissues of the endometrium or lining of the uterus. Symptoms typically associated with this type of cancer include vaginal bleeding and pelvic pain.
Former “Howard Stern Show” co-host and actress Robin Quivers, 71, is a resilient fighter who managed to beat stage 3 cancer and the hair loss condition alopecia. Stern finds her incredibly inspirational for maintaining a positive attitude as she faces arduous health challenges.

Quivers is a Baltimore native who earned several movie credits during the ‘90s, including “Private Parts,” an autobiographical story about famed radio host Howard Stern. However, her connection to Stern gained her the most notoriety as his co-host on his popular radio show from 2010 to 2013.
Read More
“Your positive attitude and the way you tackle various health challenges…most of us would crumble,” he continued.
Expert Resources to Help Patients Living With Endometrial Cancer
- ‘The Google Earth of Endometrial Cancer’ — a New, Molecular Snapshot Could Lead to Better Treatment of the Disease
- Advanced or Recurrent Endometrial Cancer Patients Have New Hopeful Combination Therapy Option
- Combo Immunotherapy-Chemo Treatment May Help Slow Progression of Advanced Endometrial Cancer: Studies Show Promising Results
- Hope for Endometrial Cancer: FDA Approves Durvalumab/Chemotherapy Combination for Hard-to-Treat Advanced Disease
Robin’s Cancer Journey
Quivers’ cancer journey began in 2012 when she was diagnosed with endometrial cancer.
Endometrial cancer begins when cancerous cells form in the tissues of the endometrium or lining of the uterus, according to the National Cancer Institute.
After a woman has been diagnosed with endometrial cancer, her doctor will stage the cancer based on its spread within the body. A pelvic exam and imaging tests help your doctor learn if the cancer has spread or metastasized.
Some common risk factors for endometrial cancer include:
- Obesity
- Taking estrogen-only hormone replacement therapy after menopause
- Having never given birth or started menstruation at an early age
- Having a family history of endometrial cancer
As for Quivers, her diagnosis was not a straight line.
“Nobody was able to diagnose it,” she told People Magazine.
Her symptoms began after she started having trouble urinating and feeling more fatigued. She went to the doctor to get some answers, and her CT scans, MRIs, and biopsies remained inconclusive. Quivers described the period of uncertainty as “scary” and “bizarre.”
Further tests finally found the culprit, a grapefruit-size mass on “every organ in her pelvic area.”
Following the discovery, a hysterectomy was ordered, and the popular radio host underwent the procedure.
A hysterectomy is a procedure that removes part or all of the uterus (or womb), often along with the cervix, according to the National Cancer Institute. Women who receive a diagnosis of uterine, ovarian, and cervical cancer may have their cancer treated with a hysterectomy.
Following the procedure, Quivers began chemotherapy and radiation treatments that spanned 15 months.

“When you’re in and out of treatment, you’re always recovering and trying to get back to where you were,” Quivers said.
After undergoing intensive treatment, Quivers reached remission, which lasted for more than three years. Then, in late 2016, she experienced a relapse and needed additional treatment after the cancer returned and metastasized to her lymph nodes. After getting her cancer under control, she undergoes immunotherapy infusions periodically.
The immune system uses its white blood cells to attack abnormal or foreign cells in the body. Cancerous cells can prevent the immune system from doing its job and attacking foreign cells. Cancer produces certain proteins that protect the tumor from white blood cells. As a result, the body does not recognize the tumor as abnormal. However, immunotherapy treatments stop this from happening and ensure that the white blood cells recognize the cancer cell properly and attack it.
Today, Quivers says she feels fine.
Coping With Hair Loss
Quivers previously dealt with alopecia prior to undergoing cancer treatment.
According to research published in JAMA, “alopecia areata is an inflammatory disease of the follicular unit that results in nonscarring patches of hair loss occurring on the scalp, eyebrows, eyelashes, and beard area.”
The condition tends to impact Black and Hispanic populations than white populations.
When you compile alopecia with the chemotherapy side effect of hair loss, Quivers was faced with this emotional stage of the cancer journey with added force.
“Your hair doesn’t fall out the way you think it’s going to fall out. It falls out in patches. It becomes this horror story,” Quivers said on an episode of the Howard Stern Show from September 2013.
“I had a barber shave my head the first time and teach me how to do it, and as soon as he was done, I said, ‘Is there anything about my head that should not be seen?” light-heartedly.
WATCH: Hair loss during chemo.
Hair loss is challenging for women and men alike, but it can be incredibly difficult for cancer patients. Losing your hair or seeing it thinning is a common side effect of some cancer treatments.
Chemotherapy can cause hair loss. It usually begins about three to four weeks after starting chemotherapy and continues throughout treatment.
It happens because this treatment targets quickly dividing cells throughout the body. That includes cancer cells but also hair cells.
“For cancer patients, losing one’s hair can be unbelievably stressful. To start with, the dread of losing one’s hair can lead to some sleepless nights and feelings of anxiety,” Dr. Samantha Boardman, a New York-based psychiatrist and author, told SurvivorNet.
To better cope with this emotional stage of the journey, Dr. Boardman suggests reaching out to other survivors who have been through a similar situation.
Radiation is another treatment that can lead to hair loss if the hair is in the path of the tumor being treated. Radiation for a brain tumor, for example, may cause hair loss.
“If you do lose hair, it will regrow several weeks or months after treatment,” radiation oncologist Dr. James Taylor told SurvivorNet.
“Fortunately, for most patients, hair loss is not a concern when having radiation therapy,” Dr. Taylor continued.
Fortunately, hair loss during cancer treatment is not all bad news. Most people can expect regrowth four to six weeks after treatment. However, when your hair grows back, you may notice some changes in its color and texture.
If losing your hair is a concern for you before cancer treatment, know you have options like wigs, hats, wraps, and scarves, among other things.
Another option that can minimize hair loss is cryotherapy, “just a fancy way for saying cold therapy,” says Dr. Renata Urban, gynecologic oncologist at the University of Washington in Seattle.
Cryotherapy involves wearing cold caps or special cooling caps before, during, and after each chemotherapy treatment.
WATCH: What is a scalp-cooling device?
The caps, which are tightly fitting and strap-on helmet-style, are filled with gel coolant chilled to negative (-15) to (-40) degrees Fahrenheit.
The caps “cause vasoconstriction, or a narrowing of the blood vessels bringing blood to the scalp,” Dr. Urban explains. By constricting the blood flow to the scalp, the caps limit the amount of circulating chemotherapy that reaches the hair follicles, protecting them from some of the chemo’s damaging effects.
The cold also decreases the activity of the hair follicles, slowing down cell division and making them less affected by chemotherapy medicine.
“This has been shown to reduce hair loss by 50 percent,” Dr. Urban says. “I do try to let patients know it’s not a 100 percent prevention strategy, and it’s not been studied in all hair types, but it is at least an available strategy for patients to try.”
Keep in mind you will be experiencing some cold temperatures. Some women find the caps give them a headache. To help withstand the chilly temps, some women will dress warmly and bring blankets.
Of course, always talk with your doctor about potential treatments to mitigate the loss and the resources you have available to handle it.
Better Understanding Endometrial Cancer and Treatment Options
In recent years, endometrial cancer patients have seen an increasing number of treatment options emerge to make battling the disease more manageable.
WATCH: New Combination Therapy for Advanced Endometrial Cancer Patients
The impact of new combination therapies on advanced endometrial cancer – a type of cancer that affects the lining of the uterus – is a significant advance for treating the disease. Patients are living longer, healthier lives.
Durvalumab (brand name IMFINZI) is an immunotherapy drug that’s often used alongside chemotherapy.
Olaparib (brand name LYNPARZA) is a PARP inhibitor, a type of drug that helps treat some cancers by blocking an enzyme called PARP that helps repair damaged DNA in cells. Olaparib destroys cancer cells, especially cells that already have trouble repairing their DNA. Sometimes, it’s used as an add-on to durvalumab.
“For a long time, patients with early-stage endometrial cancer generally do very well with a combination of surgery, maybe some radiotherapy,” says Dr. Shannon Westin, a professor in the Department of Gynecologic Oncology and Reproductive Medicine at the University of Texas, MD Anderson Cancer Center in Houston, TX.
“However, there’s a population of patients that are diagnosed at a later stage, stage three or four, or that have their cancer come back after initial therapy. And those patients have had a really hard time,” she adds.
According to Westin, the latest treatments combine immunotherapy with standard chemotherapy plus a drug that prevents cancer cells from fixing their own DNA.
The results are encouraging, especially for patients who have late-stage endometrial cancer or whose disease has come back.
Some known side effects of durvalumab and Olaparib include:
Durvalumab can cause inflammation in various parts of the body, which can lead to:
- Skin rashes
- Diarrhea
- Liver inflammation
Olaparib may lead to side effects such as:
- Fatigue
- Nausea
- Blood-related issues such as anemia
- Increased risk of developing certain other cancers due to the DNA repair inhibition.
Another U.S. Food and Drug Administration (FDA) approved combination therapy for advanced or recurrent endometrial cancer to be used with traditional chemotherapy is dostarlimab-gxly (brand name Jemperli). It is an immune checkpoint inhibitor, a type of immunotherapy that helps reinvigorate the body’s immune system to fight cancer.
WATCH: Treatment for Advanced or Recurrent Endometrial Cancer
Dostarlimab-gxly was already approved for metastatic and recurrent endometrial cancer in cases where chemotherapy did not work. Now, dostarlimab-gxly is approved as part of the first treatment for patients who have a specific set of genetic mutations called mismatch repair deficiency (dMMR) or microsatellite instability-high (MSI-H). These genetic factors are associated with a much greater response to the check-point inhibitor class of drugs.
Questions for Your Doctor
If you have been diagnosed with endometrial cancer, you may want to ask your doctor a few questions to ensure you are well informed about your diagnosis and the treatment journey that awaits.
- What stage is my endometrial cancer?
- What are the treatment options available for my specific type and stage of endometrial cancer?
- What are the potential side effects of each treatment option, and how can they be managed?
- What is the expected prognosis for my condition?
- Are there any clinical trials or experimental treatments that I may be eligible for?
- How often will I need follow-up appointments and tests to monitor my condition?
- Are there any lifestyle changes or dietary recommendations that can help improve my prognosis or manage side effects?
- What support services are available to help me cope with the emotional and practical aspects of living with endometrial cancer?
Learn more about SurvivorNet's rigorous medical review process.

