Remembering Alex Trebek & His Perseverance
- Beloved “Jeopardy!” host Alex Trebek passed away one year ago after a year-long battle with stage 4 pancreatic cancer. Now he’s being remembered by his former producer for his determination to continue working through “much pain”.
- Trebek remained the host of the TV trivia show, while keeping his viewers up to date on his progress amid undergoing treatment. He was also extremely open about the side-effects he experienced as a result of chemotherapy, and how it affected his mental state significantly at times. Trebek later turned to an experimental therapy, developed by Dr. Patrick Soon-Shiong, which attempts to use multiple parts of the immune system to destroy tumors.
- Palliative care is a type of care that’s meant to address the symptoms and side effects that your cancer or its treatment. Examples of these symptoms may include psychological experiences like stress and fear to physical experiences like pain and discomfort. The National Cancer Institute (NCI) defines palliative care as “an approach to care that addresses the person as a whole, not just their disease.”
- Studies have shown that palliative care, which encompasses many different support services from symptom management to emotional support and financial help can be incredibly helpful when it’s incorporated at the start of your cancer journey.
Trebek had battle stage 4 pancreatic cancer and remained the host of the TV trivia show, while keeping his viewers up to date on his progress amid undergoing treatment.
Read More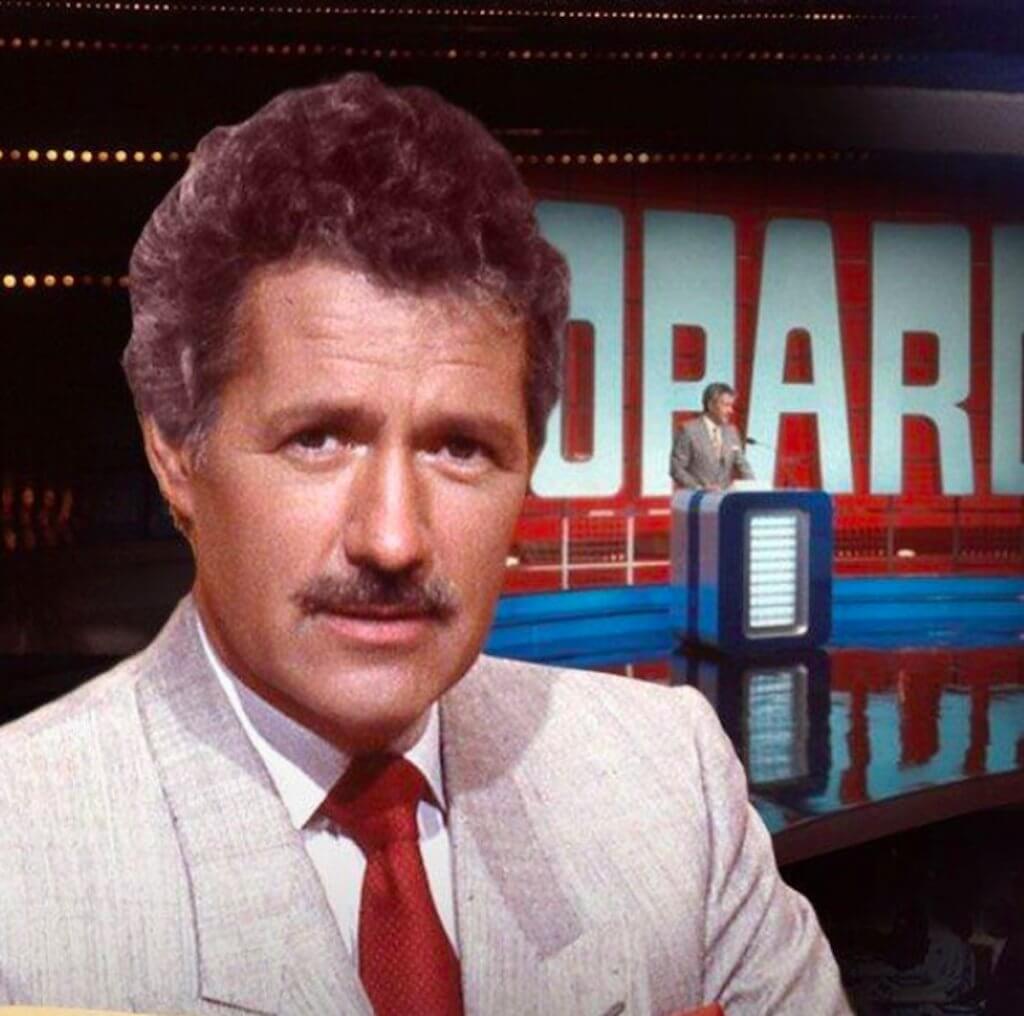 RELATED: Alex Trebek’s Transparency About Pancreatic Cancer Battle Caused “Tremendous Spike” In Awareness & Helped Many Understand the Disease Now, nearly four years after the Canadian-American TV host and personality passed, Richards is looking back on Trebek’s 20-month-long, and painful cancer fight.
RELATED: Alex Trebek’s Transparency About Pancreatic Cancer Battle Caused “Tremendous Spike” In Awareness & Helped Many Understand the Disease Now, nearly four years after the Canadian-American TV host and personality passed, Richards is looking back on Trebek’s 20-month-long, and painful cancer fight.Speaking exclusively to People, Richards, known for hosting “Let’s Make a Deal,” said, “I don’t think I will ever see anything like it again. I’ve never seen someone in that much pain or that ill in my life, let alone going out and pitching five perfect games a day.”
Richards, 48, had once replaced the late Trebek as a host for one day in August 2021 but was ultimately fired, recounted to the celebrity news outlet, “We never talked to potential hosts to replace Alex once we knew he was sick.
“A conversation like that would have been so disrespectful.”
He added, “But we had talked about people coming in and guest hosting if Alex got too sick, but we always knew Alex would come back until the day he decided he couldn’t.”
Trebek had been the face of “Jeopardy” from the year 1984 until his passing in 2020. His tenure spanned 37 seasons or roughly 8,000 episodes. The show itself was created by fellow cancer warrior Merv Griffin who bravely battled prostate cancer.
View this post on Instagram
Trebek loved his job was determined to do his job despite the amount of pain he was in. In fact, last year, “Jeopardy!” producer Rocky Schmidt opened up to Fox News about the TV host’s noticeable struggle.
Schmidt said, “When he was sick and taking medication, the pain the man had, you could watch him and it’s like ‘he’s not going to make it to the conference room table.'”
However, Trebek pushed through his lingering health challenges, and inspired those around him with his fighter’s spirit, ultimately deciding to reveal his diagnosis with his colleagues.
“Alex called and told us he had stage 4 pancreatic cancer. Alex, from the very beginning, said, ‘This is not going to affect anything,'” Schmidt recalled.
Alex Trebek’s Cancer Battle
Alex Trebek died of pancreatic cancer after a year and a half of battling pancreatic cancer, an aggressive form of cancer. While some celebrities choose to keep their cancer battles private, the “Jeopardy” star openly spoke about his treatment process with the public, and in doing so, educated millions on the disease.
While hosting an episode of “Jeopardy!” in March 2019, Trebek shared with fans that he had been diagnosed with stage 4 pancreatic cancer, and would immediately start pursuing treatment.
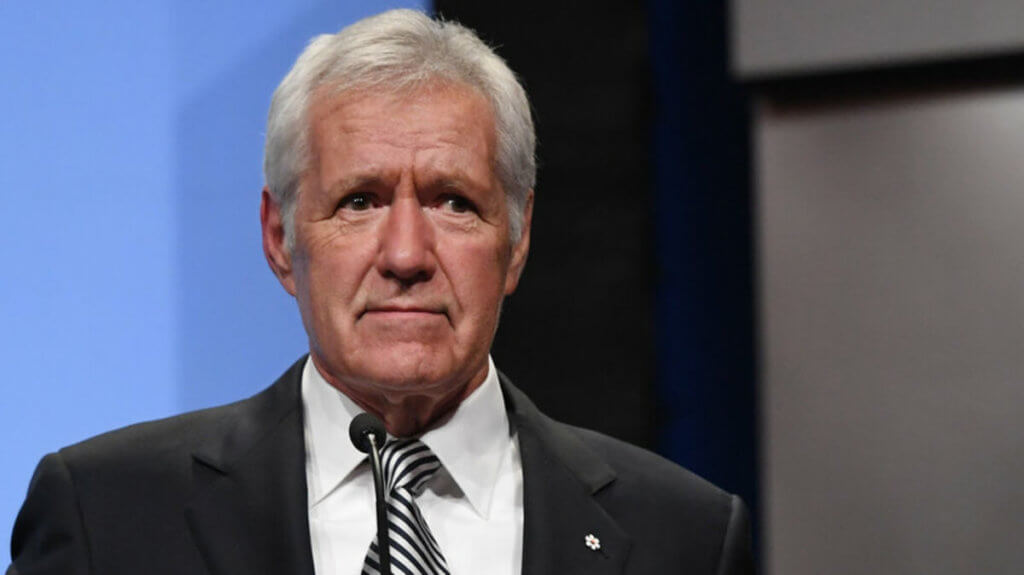
Despite the difficult journey, he remained the host of the TV trivia show and would keep viewers up to date on his progress periodically. At the time of his diagnosis, the one-year survival rate of pancreatic cancer was just 18%, but in June 2020 he made a special announcement that he’s “beating the odds” by surpassing the one-year-survival rate.
In addition to sharing good news, Trebek was also extremely open about the side-effects he experienced as a result of chemotherapy, and how it affected his mental state significantly at times. He later turned to an experimental therapy, developed by Dr. Patrick Soon-Shiong, which attempts to use multiple parts of the immune system to destroy tumors.
Trebek’s transparency made a huge impact in educating the public on pancreatic cancer, and made people more vigilant in spotting symptoms early.
In fact, one “Jeopardy!” viewer said Trebek “saved his life” when the TV show host shared symptoms he experienced before his diagnosis, and the viewer realized he was also experiencing these symptoms. As a result, the viewer’s pancreatic cancer was caught at an early and treatable stage.
Learning about Pancreatic Cancer
Pancreatic cancer is an aggressive disease that is difficult to detect because symptoms, including jaundice and weight loss, typically present at a later stage in the cancer’s development. In a previous interview with SurvivorNet, Dr. Anirban Maitra, the co-leader of the Pancreatic Cancer Moon Shot at MD Anderson Cancer Center, explains what he typically sees when patients develop this disease.
“Because the pancreas is inside the abdomen often doesn’t have symptoms that would tell you that something is wrong with your pancreas,” he says. “By the time individuals walk into the clinic with symptoms like jaundice, weight loss, back pain or diabetes, it’s often very late in the stage of the disease.”
Detecting Pancreatic Cancer Early Is Crucial
Parents, siblings and children of someone with pancreatic cancer are considered high risk for developing the disease because they are first-degree relatives of the individual. PGVs (pathogenic germline variants) are changes in reproductive cells (sperm or egg) that become part of the DNA in the cells of the offspring. Germline variants are passed from parents to their children, and are associated with increased risks of several cancer types, including pancreatic, ovarian and breast cancers. Germline mutations in ATM, BRCA1, BRCA2, CKDN2A, PALB2, PRSS1, STK11 and TP53 are associated with increased risk of pancreatic cancer.
Jessica Everett, a genetic counselor at NYU Langone’s Perlmutter Cancer Center, encourages people in this category to look into possible screening options.
“If you’re concerned about pancreatic cancer in your family, start by talking to a genetic counselor to learn more about your risk and what options you have,” Everett previously told SurvivorNet.
In addition, note that up to ten percent of pancreatic cancer cases are caused by inherited genetic syndromes. So, if two or more members of your family have had pancreatic cancer, or if you have pancreatic cysts, it’s worth asking your doctor to check for pancreatic cancer since you’re at high risk.
Dr. Allyson Ocean explains why pancreatic cancer is so hard to treat.
Understanding Palliative Care & Pain Management
During palliative care, the patient is provided specialized medical care as they manage symptoms associated with their medical condition. This form of care may also provide treatment “intended to cure” the illness.
RELATED: What You Need to Know About Pancreatic Cancer
The National Cancer Institute (NCI) describes palliative care as something that’s “meant to improve the quality of life of patients who have a serious or life-threatening disease, such as cancer.”
“It can be given with or without curative care. Palliative care is an approach to care that addresses the person as a whole, not just their disease. The goal is to prevent or treat, as early as possible, the symptoms and side effects of the disease and its treatment, in addition to any related psychological, social, and spiritual problems,” the institute explains. “Patients may receive palliative care in the hospital, an outpatient clinic, a long-term care facility, or at home under the direction of a licensed health care provider. Anyone can receive palliative care regardless of their age or stage of disease.”
WATCH: Palliative care improves your overall treatment by focusing on comfort.
“It’s not the same thing as hospice. It’s really important to recognize that palliative care, whether provided by your oncologist or by a specialty palliative care team, is an important adjunct to your oncologic care,” Dr. Lisa Diver, a gynecologic oncologist and Medical Director at ImmunoGen tells SurvivorNet.
Dr. Diver continued, “It doesn’t mean that your doctor is going to stop treatment or even wants to talk about that, but simply that he or she thinks it’s important to support all aspects of your health. That could be pain control, [relief for] nausea or constipation, or mental health care.
“All of these other symptoms that commonly arise and are intertwined inextricably with your cancer care.”
Helping Patients Better Understand Palliative Care
Research has been published showing the benefits of beginning palliative care early on in the course of treatment sometimes as soon as the initial diagnosis.
In 2016, based on results from a total of nine randomized clinical trials, one quasi-experimental trial, and five secondary analyses, the American Society of Clinical Oncology (ASCO) issued a set of guidelines stating that “inpatients and outpatients with advanced cancer should receive dedicated palliative care services early in the disease course, concurrent with active treatment.”
Some oncologists have adjusted how they talk about palliative care because of the common misconception about it compared to end-of-life hospice care.
Dr. Ishwaria Subbiah, a medical oncologist and palliative care physician at the MD Anderson Cancer Center, shared a fascinating experiment from 2009 (published in 2011): rather than trying to eliminate the deeply ingrained end-of-life connotations of the term “palliative care,” Dr. Subbiah’s colleagues at MD Anderson decided to change the name altogether, rebranding their palliative care center as the “Supportive Care Clinic.”
“We found out that the name was a big barrier to referrals,” Dr. Subbiah said. “The name itself was a barrier to accessing our services.”
Within a year of changing the name, MD Anderson’s Supportive Care Clinic saw their referrals (that is, patients coming from their medical oncologists and tumor-directed cancer treatment to access their symptom management services) rise 41 percent. “And it has been consistently increasing in the double digits ever since,” Dr. Subbiah said.
Coping Mechanisms for Pain Management
According to the Centers for Disease Control and Prevention, 20% of Americans are living day-to-day with chronic pain.
The National Institutes of Health (NIH) is conducting basic pain research to develop strategies and potential medications to better manage pain. The research focuses on key areas including facial pain and how – in some cases – protein increases sensitivity to painful and nonpainful stimuli.
RELATED: Clinical Trials Can be Life-Saving for Some
Research involving mice indicates that rodents with high levels of Cdk5 (a type of protein called cyclin-dependent kinase 5) showed larger calcium surges, indicating that their pain responses were intensified.
“This heightened pain sensitivity is similar to a condition called allodynia. Allodynia causes pain in response to something that isn’t typically painful. The research team was able to reduce pain signaling in those oversensitive mice by blocking their Cdk5,” NIH Distinguished Investigator Dr. Kenneth M. Yamada explained.
Other areas of research include learning how sound reduces pain and ongoing clinical trials studying pain perception and lower back pain.
Of course, pain management comes with risks especially when powerful painkillers such as opioids are involved. The Centers for Disease Control and Prevention recommends seeking treatment opinions that don’t involve opioids to treat pain when viable. Medicines like over-the-counter painkillers including acetaminophen, ibuprofen, and naproxen have fewer side effects. Other alternatives to opioids include physical therapy and exercise.
Questions for Your Doctor
If you are in the middle of your cancer journey, or caring for a loved one who is asking questions about late-stage care can be helpful. To help you begin your conversation, consider the following questions.
- How will I know if I need palliative care to aid my cancer treatment?
- How does palliative care differ from the care I’m getting now?
- Who provides palliative care?
- Will my insurance cover palliative care?
- Is there a moment when palliative care becomes hospice care?
Living with Cancer
Life doesn’t slow down for a cancer diagnosis, but that doesn’t have to be a bad thing. Like we’ve seen in the case of Trebek, it’s important to remember that a cancer diagnosis does not mean the end of your life. In fact, our experts say that prioritizing your overall wellbeing and continuing to do the things that you love can be very beneficial because studies have shown that patients who are able to stay upbeat and positive often have better treatment outcomes.
According to Dr. Dana Chase, a gynecological oncologist at Arizona Center for Cancer Care, it doesn’t even really matter what you do as long as it makes you happy. So, if that means continuing to host “Jeopardy” like Trebek did until shortly before his passing, then that’s exactly what you should do.
Dr. Dana Chase encourages those facing cancer to find moments of joy during treatment
“We know from good studies that emotional health is associated with survival, meaning better quality of life is associated with better outcomes,” Chase previously told SurvivorNet.
“So working on your emotional health, your physical well-being, your social environment [and] your emotional well-being are important and can impact your survival. If that’s related to what activities you do that bring you joy, then you should try to do more of those activities.”
Meanwhile, Sarah Stapleton, a clinical social worker at Montefiore Medical Center, previously told SurvivorNet, “We always encourage people to continue to work if they can. I think it creates a sense of normalcy for patients.”
If you’re able to work, you’ll be busy, and you may not be worrying all the time about how your treatment is going, Stapleton adds.
Sometimes, cancer can make you feel isolated and lonely, and being around people for work can alleviate feelings of loneliness.
It would be best to talk with your doctor before continuing to work during treatment. Ask your physician what you can and cannot do so you don’t disrupt ongoing treatment.
Remember, sometimes cancer treatment can cause fatigue, leaving you unable to fulfill your duties as you once could. Fortunately, some on-the-job accommodations can make working during cancer treatment much easier.
WATCH: Choosing to Work During Cancer Treatment
It’s important to know that The Rehabilitation Act or the Americans with Disabilities Act protects people with job problems related to cancer. The Family and Medical Leave Act (FMLA) may also benefit others. This law allows many people with serious illnesses to take unpaid leave to get medical care or manage their symptoms.
Your human resources department should be able to share with you your options.
In some situations, employers must accommodate a qualified applicant or employee with a disability unless the employer can show it would be an undue hardship to do so. This could mean making changes to work schedules, equipment, or policies.
Laurie Ostacher, a behavioral health clinician at Stanford Health Care, recommends that cancer patients discuss accommodations they may need upon returning to work with their employers.
“Patients need to let their employer know [they’re] going to need some flexibility… Because there are going to be days when you’re not as energetic or feeling as well as other days,” Ostacher explained.
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.

