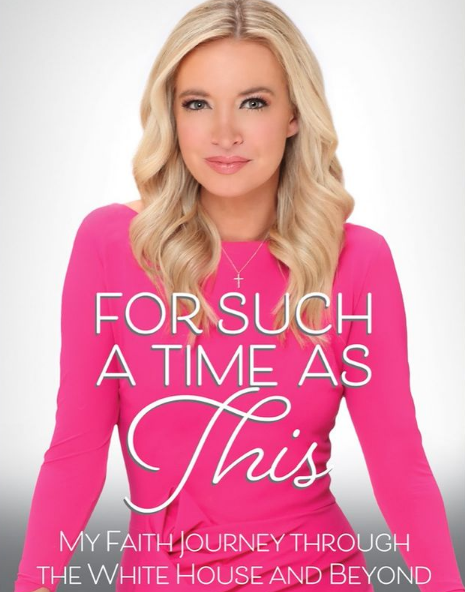
Kayleigh McEnany On Choosing Routine Surveillance Over Surgery
- Fox News host Kayleigh McEnany learned she had the BRCA gene mutation, which put her at a higher risk of being diagnosed with breast cancer while still in college. She chose to get tested after her mother’s 2009 preventative double mastectomy.
- The former White House spokesperson chose routine surveillance over a double mastectomy for the next ten years, writing in her new memoir that she feared what it would be like dating after having a double mastectomy while still in her twenties.
- Experts say BRCA1 or BRCA2 are mutations identified in less than 10% of women with breast cancer. You can be born with the mutation or acquire it over time.
In her new memoir, the former White House spokesperson, 33, reveals that she tested positive for the BRCA gene while still in college, having decided to find out her risk factor after watching her mother undergo a preventative double mastectomy in 2009.
Read More
“Initially, I set out to get the same surgery as my mom,” writes McEnany in her memoir, an excerpt of which appears on FoxNews.com.
“I wanted to do it fairly quickly. Within the year, I had hoped. But I was single at the time. I wasn't sure what dating post-mastectomy would be like, and the unknown worried me.”
McEnany says she knew that her risk of breast cancer would be relatively low until she reached the age of 30, leading her to choose routine surveillance over surgery.

“Every six months, I would go to Moffitt Cancer Center and receive either a mammogram or an MRI,” explains McEnany. “Mammograms were often followed by an ultrasound since it was hard to see through my dense breast tissue.”
McEnany recalls how at her first screening, a woman in the waiting room informed her that she should not worry unless the doctor called her back for an ultrasound, just moments before the doctor did just that. However, it turned out that McEnany’s dense breast tissue meant that most screenings would involve an ultrasound in addition to a mammogram.

In between screenings, McEnany would also perform self-exams. If she felt anything that could be a reason for concern, she would have it immediately examined by her OBGYN or someone in the area when she could not get an appointment with her oncologist.
Her decision to have a double mastectomy never changed, though, and six months after marrying major league baseball player Sean Gilmartin ​in 2017, she went in for surgery.
“On that day, nearly ten years after my diagnosis, I decided to have the same surgery as my mom,” writes McEnany. “A big reason I had the confidence to make this decision was that I had found a supportive husband in Sean Gilmartin.”
McEnany writes of the myriad emotions she experienced in the lead-up to her surgery and her surprise when she woke up after her procedure.
“When they unveiled my dressings to reveal my breasts, I proclaimed with amazement, ‘Did they even do the surgery?! The nipple-sparing procedure and implants in place left me looking almost the same,” recalls McEnany.
“I still looked like me. More importantly than that, like my mom, I could now say with confidence that I would never die of breast cancer.”
McEnany credits her family and faith with her helping her through the journey but notes that two women, in particular, gave her strength during her time of need.
She thanked those two women while writing in the journal she kept documenting her journey.
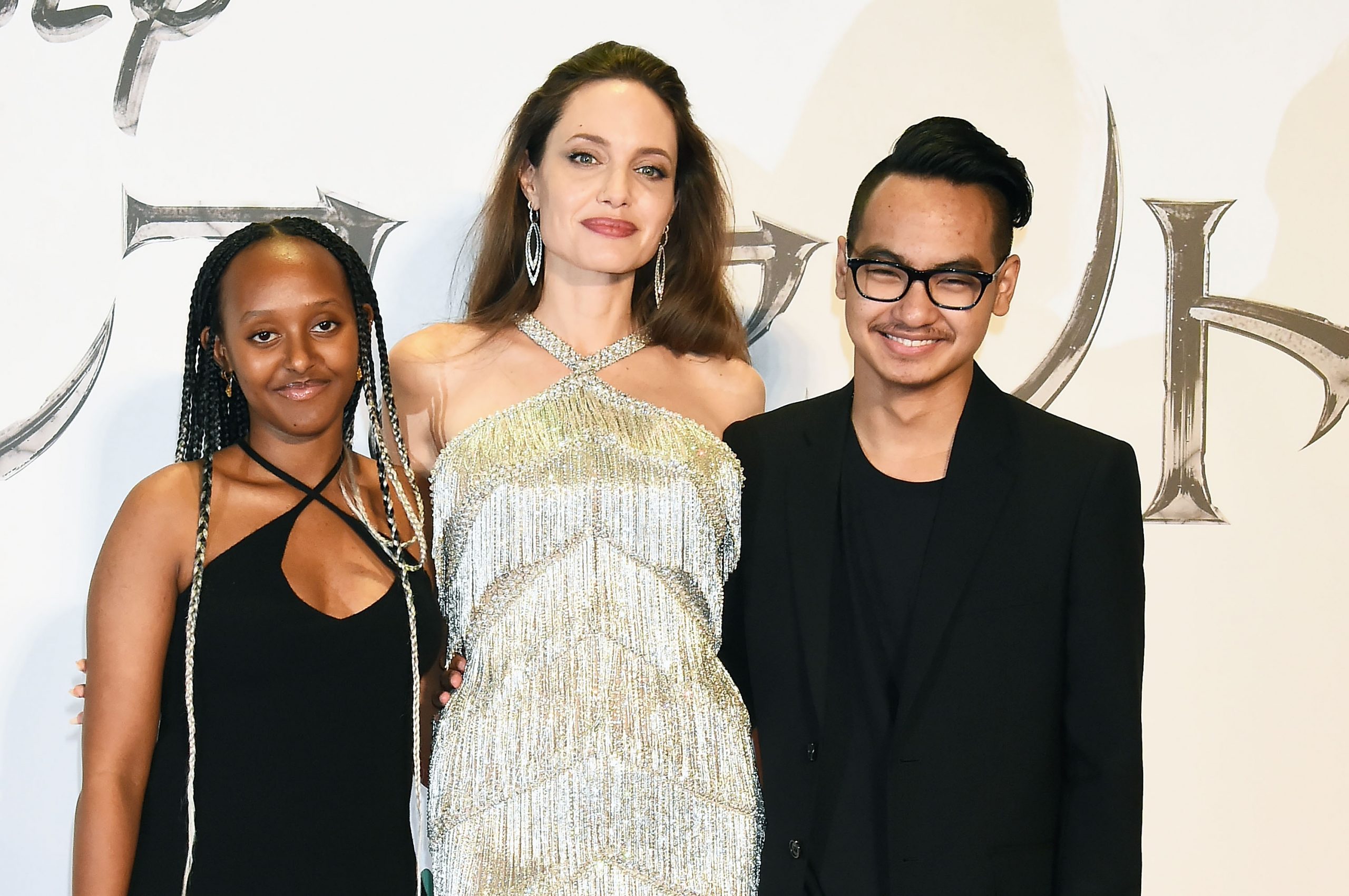
“Women like Angelina Jolie, who wrote about her decision to have a preventative mastectomy. And women like my mother, who boldly took this step without hesitation,” wrote McEnany. “Their strength has become my own. It was important for me to share this with you for a very simple reason: this day was only made possible because of these women who so openly and publicly shared their experiences.
Jolie revealed in a 2013 New York Times op-ed that she had a preventative mastectomy after learning she had the BRCA gene, explaining her decision to undergo the procedure by writing: “I can tell my children that they don't need to fear they will lose me to breast cancer.”
A double mastectomy is not the only preventative surgery McEnany plans to undergo either, as she told SurvivorNet in an interview earlier this year.
McEnany, who welcomed a daughter Blake in 2019, said that a preventative hysterectomy is "certainly the plan, probably in my 40s" due to her increased risk of ovarian cancer.
She noted, however, that she would like to first have three of four kids before then and possibly even adopt a child “if it ever fit into our life.”
For Such a Time as This: My Faith Journey will be available in December.
What Is A BRCA Mutation?
Kayleigh McEnany is a perfect example of a previvor, using frequent screening and then surgery to prevent her risk of breast and ovarian cancer.
Both she and her mother managed to avoid the disease that McEnany writes “plagued” many others in her life, including eight aunts and cousins on her mother’s side of the family.
That family history is also why she tested to see if she had the BRCA gene mutation. Dr. Heather McArthur, clinical director of breast oncology at the Simmons Comprehensive Cancer Center at UT Southwestern Medical Center, previously told SurvivorNet that it is two gene mutations that McEnany and others are being tested for at the time.
“So BRCA mutations, either BRCA1 or BRCA2, are mutations identified in less than 10% of women with breast cancer,” noted Dr. McArthur. “They’re mutations that one can be born with or one can acquire over time. ”
Dr. McArthur explained that these mutations are common in some forms of breast cancer.
“BRCA mutations and triple-negative breast cancer go hand-in-hand,” pointed out Dr. McArthur. “There’s a higher incidence rate of triple-negative breast cancer for patients with BRCA mutations.”
What Is A BRCA Mutation?
Advancements In Battling Breast Cancer
Kayleigh McEnany is one of the increasing numbers of young women and men who choose to be proactive in learning if they have the BRCA gene mutation.
The good news for these individuals is that there have been several advancements in recent years for women who do and have gone on to get cancer.
“One of the most interesting or promising developments [recently] was a drug called olaparib, which comes from a class of drugs called PARP inhibitors,” said Dr. McArthur.
Sold as Lynparza and approved by the Food and Drug Administration, the PARP inhibitor treats women with metastatic breast cancer with BRCA-mutation, carrier-related breast cancers.
“PARP inhibitors also interfere with DNA repair,” explained Dr. McArthur. “So in people who already have a DNA repair defect, [introducing a PARP inhibitor] to further impair redundant repair mechanisms has been a successful strategy.”
It works, said Dr. McArthur, because “PARP inhibitors undermine those redundant mechanisms so that [patients] don’t have the backup opportunity for DNA repair.”
A 2017 study published in the New England Journal of Medicine showed how well the PARP inhibitor worked in patients with the BRCA mutation.
“Among patients with HER2-negative metastatic breast cancer and a germline BRCA mutation, olaparib monotherapy provided a significant benefit over standard therapy; median progression-free survival was 2.8 months longer, and the risk of disease progression or death was 42% lower with olaparib monotherapy than with standard therapy,” wrote researchers.
The group arrived at that conclusion following the results of a clinical trial with just over 302 participants.
Who Can Have PARP Inhibitors?
Learn more about SurvivorNet's rigorous medical review process.


