Von-Hippel Lindau (VHL) disease is a rare condition that is caused by a mutation on the VHL gene. The disease is lifelong, with many patients experiencing numerous tumors throughout their lifetime. The tumors associated with VHL disease can cause tumor and/or cyst growths in numerous organs throughout the body. Because of this, proper management is necessary for early identification and intervention of new growths. Management of Von-Hippel Lindau Disease involves genetic testing for a diagnosis, routine screening and surveillance for disease progression, and treatment of the disease.
Cancer Genetics
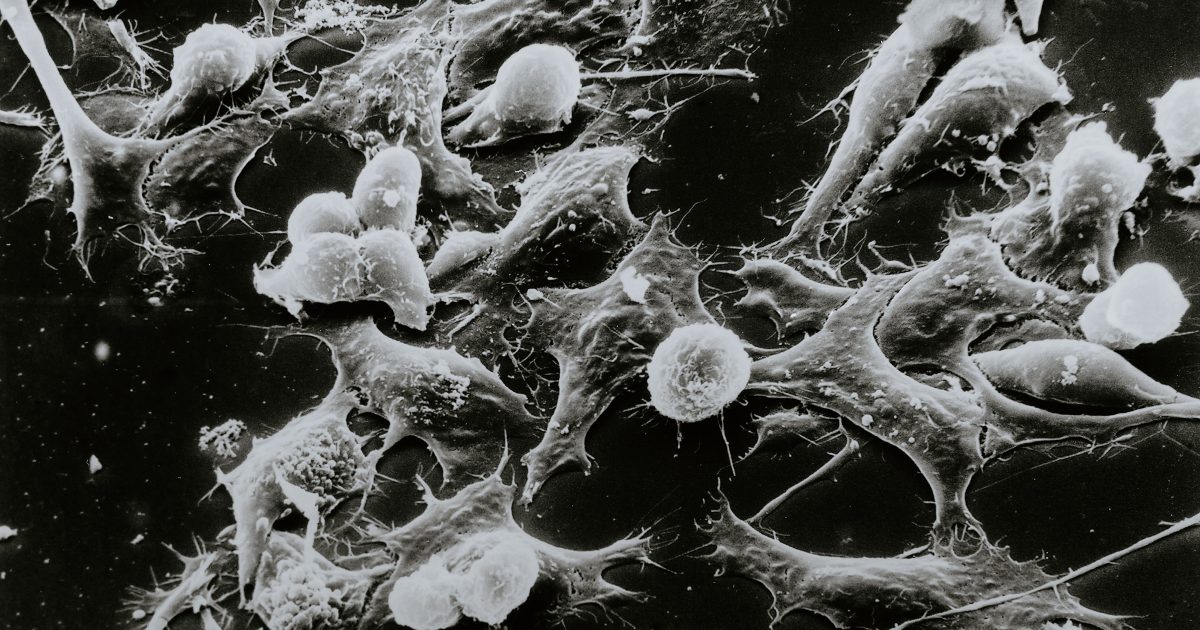
The VHL gene is a type of tumor suppressor gene. Tumor suppressor genes play an essential role in cell division. Within the body, tumor suppressor genes work to prevent cell replication and division to keep the body 'in check.' If there is a mutation in the gene, cells can rapidly divide and multiply, resulting in tumor growth and proliferation.
Read MorePrognosis Meaning
The VHL Alliance reports that 97% of patients will have one or more tumors by the time they are about 65 years old. At face value, this number seems high. However, it is important to recognize the prognosis is different for each and every patient. Although all patients diagnosed with VHL disease have a mutation on the VHL gene, not all patients will have tumor growth, and a minority may not have a disease-causing variant of the gene.The prognosis of VHL disease is dependent on many factors, such as the size, location, and type of tumor. The most common tumors that can develop because of VHL disease include:
- Hemangioblastomas
- Renal Cell Carcinoma
- Pheochromocytoma and Paragangliomas
- Endolymphatic Sac Tumors
- Pancreatic Endocrine Cysts and Tumors
- Cystadenomas of the Epididymis and Broad Ligament
According to the National Institute of Neurological Disorders and Stroke (NINDS), the prognosis of VHL is significantly improved if tumors are identified and treated early. Because of this, routine surveillance is a key component of the management of Von-Hippel Lindau disease.
VHL Disease Management by Tumor Type
Once a diagnosis of VHL disease is made, many different modes of surveillance are performed. Disease progression is different for each patient. With that being said, providers need to perform many different clinical procedures and exams to ensure a full-body workup is performed to identify various tumors that arise from VHL disease and identify what treatment options are available.
Management and treatment are largely dependent on which tumors and new growth are being experienced by the patient. An overview of common tumor types and specific management principles can be found below.
Hemangioblastomas
Hemangioblastomas are tumors that develop in your brain and spine within the central nervous system and within the retina of the eye. They are the most common type of tumor people with VHL experience. Hemangioblastomas are benign, meaning they do not cause cancer. However, their growth can still cause negative effects for a patient and can sometimes be deadly.
To quickly identify hemangioblastoma growth within the CNS, your clinical care team may recommend an MRI of the brain and spine every two years. This is typically performed in patients aged 11 to 65 but may also occur outside of that timeframe.
If a hemangioblastoma is found, your provider will determine if it is best to monitor growth or if active treatment or resection is warranted. In most cases, complete surgical removal is possible.
Other options for symptomatic or enlarging CNS hemangioblastomas are radiation therapy, systemic agents with a HIF-2alpha inhibitor, belzutifan (Welireg®), or antiangiogenic agents such as pazopanib (Votrient®).
For retinal hemangioblastoma prevention and management, frequent eye exams are recommended. Dilated eye exams should be performed every six to twelve months for pediatric patients and adults until the age of 30. From that point, annual dilated eye exams are a typical standard of care.
The treatment for hemangioblastoma in the eye depends on several factors, including the size and location of the tumor, if the retina is detached, or if there is scarring or any fibrosis. According to the American Academy of Ophthalmology, photocoagulation treatment may be recommended for smaller tumors, whereas cryotherapy is reserved for larger lesions.
Renal Cell Carcinoma
Patients with VHL have roughly a 40% chance of developing renal cell carcinoma (RCC). RCC is a cancer found within the kidneys. Most patients with VHL are diagnosed with a type of RCC called clear cell renal cell carcinoma, which impacts the tubules that filter out waste from the blood.
Renal Cell Carcinoma is a malignant type of tumor, and catching growth early is essential to monitoring progression and exploring all applicable treatment options. Routine abdominal MRIs may be performed every two years to monitor for any tumor growth in patients aged 15-65. If renal cell carcinoma is found, physicians will typically utilize the "3 centimeter (cm) rule" to dictate treatment. If the largest tumor found is <3 cm, your healthcare team will likely use a wait-and-see approach. This is because there is minimal potential for metastases when an RCC tumor is <3 cm. If a tumor is found to be >3 cm, or if your physician determines a tumor is growing too quickly, they may opt for the removal of part of the kidney, known as partial nephrectomy.
While surgery is the preferred modality of treatment, some patients may not be a candidate for partial nephrectomy. Nonsurgical options such as radiofrequency ablation and cryotherapy can be reasonable alternatives for those patients. Systemic therapy with belzutifan (Welireg®) can also be an option for patients who are not surgical candidates.
Pheochromocytoma and Paragangliomas
Pheochromocytoma and paraganglioma are both types of neuroendocrine tumors (NET). Paragangliomas are rare tumors found in nerve tissue. If a paraganglioma is found within the adrenal gland, it is known as a pheochromocytoma (PCC).
PCCs arise from cells within your adrenal gland called chromaffin cells, which are responsible for releasing hormones, such as norepinephrine and epinephrine. These two substances play a variety of roles in the body, including heart rate and blood pressure control. Because of this, your healthcare team will routinely monitor your blood pressure and pulse to identify any changes that may be caused by a PCC tumor.
Your provider may also order a metanephrine test. The test will determine if your body is making too much epinephrine and norepinephrine. Annual metanephrine testing is typically recommended for patients aged 5-65. Finally, routine abdominal MRIs may be performed every two years to monitor for any new tumor formation in patients aged 15-65.
Treatment options for pheochromocytomas and paragangliomas are dependent on each individual patient. According to the National Comprehensive Cancer Network, minimally invasive surgical removal is preferred if the tumor is considered resectable (easily removed by surgery). If the tumor is considered locally unresectable or metastases are found, your provider may opt to observe tumor growth if it is slow-growing and you are asymptomatic, or may recommend treatment with medication or radiation therapy.
Endolymphatic Sac Tumors
Roughly 16% of patients develop endolymphatic sac tumors (ELST). The endolymphatic sac is found within the inner ear. To monitor for tumors, your clinical care team may order a yearly hearing test, known as an audiogram, beginning at age 2 through 65 years of age. You may also undergo an MRI of your ear canal to identify any cyst or tumor growth. If an ESLT is observed, it is usually removed by minimally invasive surgery. Stereotactic radiosurgery may be an option for recurrent disease.
Pancreatic Endocrine Cysts and Tumors
Pancreatic cysts will occur in most patients, with approximately 70% of patients experiencing cysts at least once in their lifetime. Pancreatic cysts and even some pancreatic tumors known as cystadenomas can be benign (non-cancerous). Although they are benign, the size and placement of the cysts and tumors can still cause unwanted issues, such as bile duct blockages and blood sugar dysregulation.
Pancreatic neuroendocrine tumors (pNETs) are malignant tumors that can arise in patients with VHL. These tumors can be very aggressive and advance quickly. Abdominal MRIs may be performed every two years to monitor for any new cyst or tumor growth. Treatment is dependent on the type of mass found, location, and associated symptoms.
According to the American Cancer Society, resection of cysts or cystadenomas may be warranted if the patient is experiencing symptoms, or if it is unclear whether or not the mass is precancerous. Additionally, patients that have a pNET with a tumor diameter of >1.5 cm, growth between scans, or metastases may be candidates for resection (if complete resection is possible) or for systemic therapy with an HIF-2alpha inhibitor, like belzutifan (Welireg®).
Cystadenomas of the Epididymis and Broad Ligament
Papillary cystadenomas of epididymis and broad ligament are benign and generally asymptomatic. Treatment is usually not required unless the patients experience any troublesome symptoms.
Moving Forward – Questions to Ask Your Doctor
- Where can I find a VHL Clinical Care Center?
- Am I due for any routine scans or exams to monitor my VHL disease?
- What are the best treatment options for my new tumor growth?
Learn more about SurvivorNet's rigorous medical review process.