Prostate Cancer Awareness and The Importance of Early Detection
- New research, recently published in JAMA Internal Medicine, has found that older men with prostate cancer in the Veterans Affairs (VA) Health System are increasingly overtreated, especially with radiotherapy—a type of therapy late singer and actor Harry Belafonte underwent amid his battle with the disease, along with surgery and hormonal treatments.
- Although there is some debate on when men should begin prostate cancer screening, a consensus among experts is that men at average risk should begin prostate cancer screening at age 50. Men who are at higher risk should start screening at 40. Men with a close relative diagnosed with prostate cancer may want to consider annual screenings in their 30s.
- Prostate cancer behaves differently in different men. For some, it can be considered “low-risk” and slow-growing, and treatment might not be necessary. In others, the cancer may grow faster or be more aggressive, putting them in a high-risk category and calling for immediate treatment.
- There are many different treatment options for both early and later-stage prostate cancer including active surveillance, watchful waiting, surgery, radiation, cryotherapy, hormone therapy, chemotherapy, immunotherapy and targeted therapy. The disease is one where doctors may have differing opinions on the best treatment path to take, so don’t hesitate to ask lots of questions and seek out multiple opinions.
- SurvivorNet has created a comprehensive guide to help veterans diagnosed with prostate cancer better navigate the Veterans Affairs (VA) health system.
As per the cohort study, which specifically looked into 243,928 men with clinically localized prostate cancer in the U.S. Department of Veterans Affairs (VA) health system, overtreatment of the disease was found among men with limited life expectancy.
Read MoreDon’t Believe the Hype: Do Your Own Research on Prostate Cancer Treatment
Researchers said, “The fact that such overtreatment exists in a non–fee-for-service setting such as the VA (which has been a national leader in reducing overtreatment based on disease risk) suggests that the problem of overtreatment of men with limited [life expectancy] has not been solved in the active surveillance era, despite increasing numbers of men with low-risk [prostate cancer] receiving active surveillance.”
The researchers also found that more than 75 percent of the men with limited life expectancy received radiotherapy as definitive therapy, warning the finding is “critical to targeting interventions to curtail such overtreatment, and urologists and radiation oncologists need to play active roles in this effort.”
RELATED: A Step-by-Step Guide for Veterans: Seeking Care for Prostate Cancer Through the VA
It’s important to understand that prostate cancer does not always behave equally in the men it impacts. The cancer can be considered “low-risk” and slow-growing, and treatment might not be necessary. Other men, however, may have their cancer grow faster or more aggressively, requiring more immediate treatment. Because of this, there is some debate about screening.
The United States Preventive Services Taskforce recommends men at average risk between the ages of 55-69 years old should talk with their doctor about the pros and cons of prostate cancer screening.
Meanwhile, Dr. Nancy Li Schoenborn, MD, of the Johns Hopkins University School of Medicine in Baltimore, and Louise Walter, MD, of the University of California San Francisco, said as a followup to the findings, “The authors discuss multiple suggestions for reducing overtreatment by considering life expectancy during treatment decision-making, but why wait to consider life expectancy until after a prostate cancer diagnosis?
“Life expectancy should be considered during screening decision-making to reduce the number of men with limited life expectancy being diagnosed with asymptomatic localized prostate cancer in the first place.”
Overall the researchers explain that this study’s findings “suggest that despite a marked reduction in overtreatment of low-risk prostate cancer in the VA in association with adoption of active surveillance, clinicians should also avoid definitive treatment of men with limited life expectancy to prevent unnecessary toxic effects in men with insufficient longevity to benefit from treatment.”
Harry Belafonte’s Prostate Cancer Journey
The late Jamaican-American singer and actor Harry Belafonte received his prostate cancer in 1996, when he was 69 years old.
Belafonte went public with his diagnosis following his treatment, which included surgery. He then went on to become a vocal advocate for awareness, especially to those in minority communities.
In a 2004 interview with OncoLink he said, “Especially African American men, who are more prone to this disease, have to be made aware and encouraged to seek the medical attention they need and deserve.”
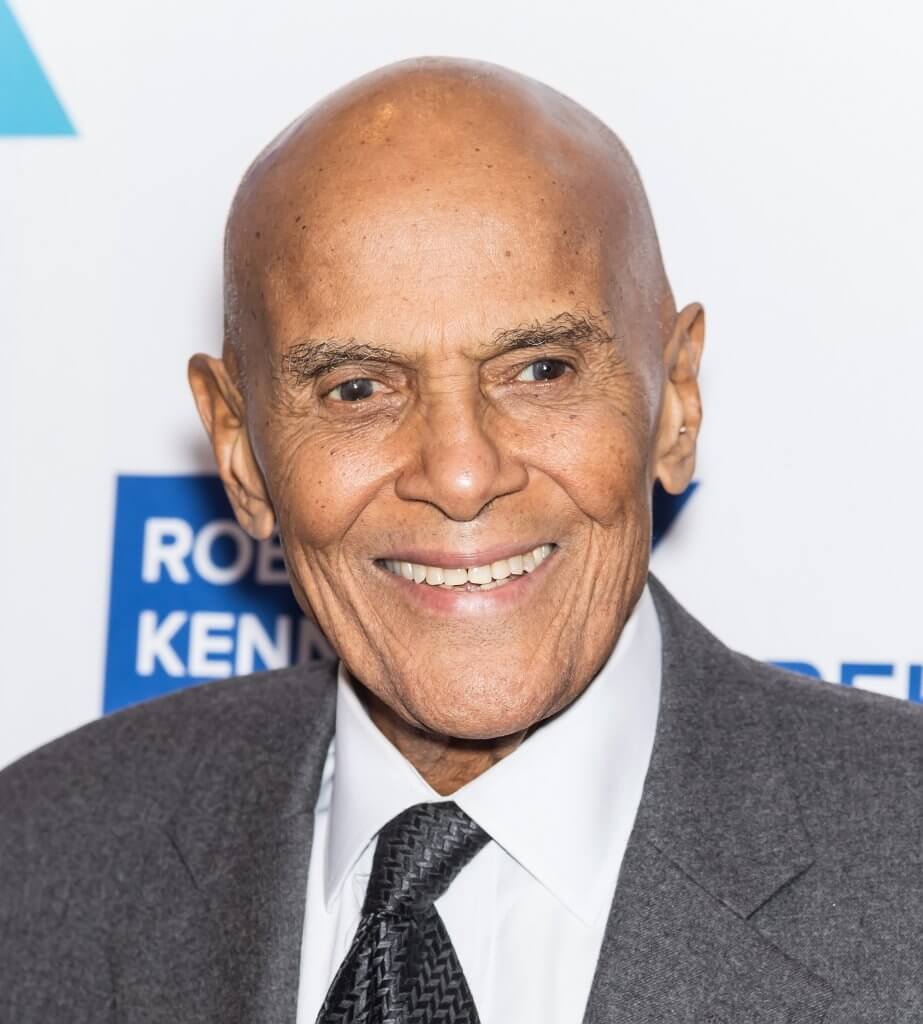
As for the fears he experienced and the decisions he had to make amid his cancer diagnosis, Belafonte told OncoLink, “When they discovered it I was very alarmed and concerned. All kinds of thoughts went through my head, like ‘why me, oh Lord? I have been a good father, a good citizen and a loving husband. Why does it have to be me?’
“I then realized that I had to make some decisions. I made a terrible mistake and did not let my family know about this diagnosis at the time. I wanted to get things settled first and decide on the therapy. I had to look very hard and very carefully into all my options.”
He continued, “Weeks of discussions with many physicians ensued. We started immediately with radiation therapy and hormonal treatments. As time passed I sought multiple opinions around the country and asked each doctor one simple question: what are the odds for each of these treatments working? Where are the highest rates of success? I listened to all the pros and cons and decided that for me the best option is really surgery.
“Since that time I have not looked back. I have been free of disease and feel that my survival is a gift. I have often asked myself how I can repay this gift and what I am meant to do. I decided that what I need to do is use my celebrity platform to encourage others to seek screening and seek treatment and to make difficult decisions like these to improve survival and wellbeing.”

Belafonte later passed away at the age of 96 on April 25, 2023, from congestive heart failure. His resilience through cancer and determination to spread awareness for the disease continues to offer inspiration for other cancer warriors.
Helping Patients Understand Prostate Cancer Treatment Options
- Deep Concern For The Nearly Half A Million Veterans Who Have Prostate Cancer: Are They Getting The Proper Treatment?
- Genetic Testing for Advanced Prostate Cancer Can Help Tailor Treatment
- How to Treat Late-Stage Prostate Cancer: New Treatment Developments
- New Drug for Advanced Prostate Cancer Gets Fast-Tracked by FDA; What You Need to Know About This Treatment
Speaking at a benefit in 1997, at the Hoag Family Cancer Institute in Newport Beach, California, Belafonte expressed the importance of decision making when it comes to battling cancer, saying, “If you’re going to have [prostate cancer], you’re going to have it.
“It’s what you do about it that makes the difference — how you conduct your life.”
Surgery Isn’t Always the First Option; Some Choose ‘Active Surveillance’
It’s common for prostate cancer to grow very slowly. Some men, especially those who are older and those who have a low risk of the cancer spreading, may not need aggressive treatment, making active surveillance a viable option.
WATCH: People With Low-Risk Prostate Cancer Can Rely on Monitoring the Disease
Active surveillance means the doctor watches the cancer carefully for changes, with a PSA blood test every six months and a digital rectal exam about once a year. You may also get prostate biopsies and imaging tests every one to three years.
SurvivorNet experts stress active surveillance is not “watchful waiting.” Active surveillance is a treatment, and as the name implies, it is active. This path requires coordination between the patient and their healthcare team.
“[It’s] not just kind of check in once a year—hey, how are you doing—but actively have a physician check a PSA and do a rectal examination,” Dr. Edwin Posadas, director of the Translational Oncology Program at Cedars-Sinai Medical Center, told SurvivorNet.
“We can actually see some of the metabolic information within the cells through our next-generation imaging and find high-risk areas that are or are not changing in a patient to let us know, yeah, that cancer’s still sleeping. Let’s not bother– let’s not put that young man through the risk of losing his sexual quality of life or his urinary quality of life,” Dr. Posadas added.
Half of men who choose this approach will avoid unnecessary treatment and potential side effects.
But the other half of men do end up having treatment, whether as a personal decision to remove the cancer or to treat the disease as it progresses. Your doctor will determine if this is necessary based on the results of your ongoing tests.
Surgery Options for Prostate Cancer
Prostate cancer treatment depends on the results of a prostate exam, your PSA numbers, and your Gleason Score, which helps determine how aggressive the cancer is.
Your doctor will determine your risk level, which ranges from low to intermediate to high. Men with low risk and very low risk may bypass surgery. Meanwhile, men at higher risk may receive more intense treatment.
WATCH: Dr. David Wise, NYU Langone medical oncologist, explains how Gleason’s score affects treatment and prognosis.
Surgery is an option for men with any risk group of prostate cancer that hasn’t spread outside of the prostate gland. The surgery procedure is called a radical prostatectomy. During this procedure, the surgeon removes the entire prostate, along with some tissue around it, including the seminal vesicles that release fluid into the semen. Your doctor can perform this through a traditional open procedure called laparoscopic surgery with one large or several small incisions.
“It’s typically done through a robotic technique today, at least in the United States, but a lot of patients are still getting open surgery,” Dr. Stephen Freedland, a urologist at Cedars-Sinai Medical Center, told SurvivorNet in an earlier interview.
“Depending on the surgeon, it may be two, three, four, five hours — somewhere in that range, usually spend one night in the hospital. You wake up from the surgery with a catheter in your bladder. Once you’re home, it’s really just recovering, gaining your strength back,” Dr. Freedland continued.
WATCH: How do you choose the right surgeon, particularly for robotic surgery?
Other common treatment options for men with prostate cancer include:
Radiation therapy.
You’ll usually get this treatment five days a week for several weeks. Newer techniques include stereotactic body radiotherapy (SBRT), which aims for more focused radiation beams at the tumor to spare surrounding healthy tissues and may allow treatment in a shorter time.
Brachytherapy implants small seeds containing radiation directly into your prostate. This type of radiation works best in men with smaller prostates.
If your prostate is very large, your doctor might give you hormone therapy first to shrink it.
Combination radiation therapy with hormonal therapy.
Androgens are male hormones that fuel the growth of prostate cancer. Androgen deprivation therapy (ADT), also known as hormone therapy, reduces levels of these hormones your body makes to slow the cancer’s growth.
“Usually, for men with tumors that spread, hormonal therapy is usually the first line that we do, and more importantly, it’s the backbone upon which we build,” Dr. Freedland explained to SurvivorNet.
Surgery followed by radiation.
Radiation therapy can be used after surgery to get rid of any cancer cells that were left behind. Getting radiation along with surgery is called adjuvant therapy.
Sometimes, men who have surgery will need radiation therapy after surgery if the surgeon cannot remove all of the prostate, your PSA does not become undetectable, or you have a high-risk genetic profile if the tissue is sent for testing.
Men with high-risk and very high-risk prostate cancer are more likely to require radiation after surgery than men with lower-risk disease.
The Side-Effects of Prostate Cancer Surgery
Prostate cancer warriors need to ask their doctor questions about the side effects of surgery.
Some of the known side effects of prostate cancer surgery include erectile dysfunction (difficulty getting or keeping an erection) and urinary incontinence (leaking urine by accident).
Treatments for prostate cancer, especially surgery, can damage nerves and blood vessels essential for erectile function, leading to ED. The risk for these side effects depends on the type of surgical approach and factors specific to your cancer.
WATCH: Sexual Function Recovery After Prostate Cancer Surgery
“Erectile function is so sensitive when we’re dealing with prostate cancer because of the fact that the nerves that are critical for this function wrap around the prostate; they’re just so intimately connected to the prostate that they can be damaged from a surgical removal of the prostate or through radiation treatment,” Dr. Isla Garraway, a staff urologist in the Veterans Administration (VA) Greater Los Angeles Healthcare System, tells SurvivorNet.
Dr. Freedland says that most people regain normal function in these areas over time.
Opting for nerve-sparing surgery can reduce this risk, though it may not suit everyone. Nerve-sparing surgery involves removing cancer without harming the nerves, but if the cancer is near the nerves, it may need removal.
Within a year of nerve-sparing prostatectomy, 40% to 50% of men are back to their pre-cancer sexual function.
For men experiencing erectile dysfunction, they should know there are plenty of solutions.
Oral medications — usually a pill — work for mild to moderate ED by enhancing blood flow to the penis to bring on an erection.
There are medications currently on the market that can aid in sustaining erections, such as Viagra, Cialis, and Levitra. There are also treatments such as penile injections and vacuum erection devices (VED), as well as the option of a penile prosthesis. Vacuum erection devices use vacuum pressure to draw blood into the penis, inducing an erection.
Dr. Freedland says there are two main prosthetic options: an inflatable prosthesis placed in the scrotum or a bendable plastic prosthesis.
According to Dr. Freedland, most men who choose this route report being pleased with the outcome.
Doctors often recommend sexual counseling after prostate cancer treatment to help improve sexual function. This approach actively addresses the psychological, emotional, and relationship impacts on sexual health.
In counseling, individuals and couples can discuss concerns, explore sexual aids and techniques, and find ways to maintain intimacy.
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.

