How a Cancer Scare Can Leave a Lasting Impact
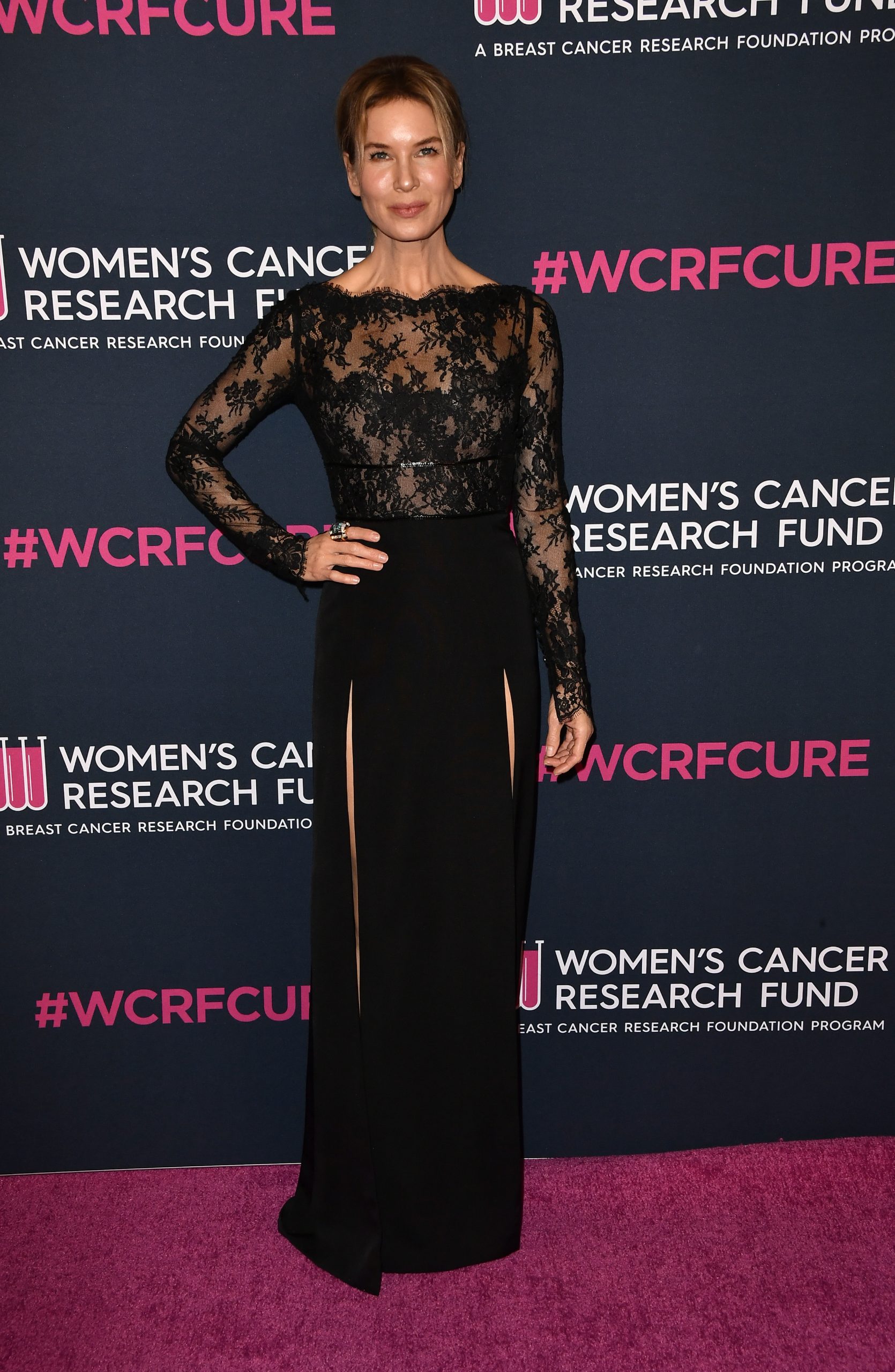
- “Bridget Jones’ Diary” actress Renee Zellweger, 55, once had a breast cancer scare after she discovered two lumps in her breasts. They turned out to be benign tumors called fibroadenomas. She had them removed to give her peace of mind.
- Fibroadenomas are among the most common benign breast tumors. These types of tumors are more common among women during reproductive age and cause no pain.
- The U.S. Preventive Services Task Force recommends women begin screening for breast cancer at age 40.
- Women with a strong family history of breast cancer, have dense breasts, have a genetic mutation known to increase the risk of breast cancer, such as a BRCA gene mutation, or a medical history, including chest radiation therapy before age 30, are considered at higher risk for breast cancer.
- While mammograms are extremely valuable for breast cancer screening, more effective screening methods like 3D mammograms and breast ultrasounds are highly recommended for women with dense breasts where fatty tissue is harder to see through on imaging scans.
- A breast cancer diagnosis can spawn a flurry of emotions and impact your mental health. To help manage your mental health while coping with a diagnosis, some helpful tips include leaning on your support group, journaling, and/or seeking a mental health professional.
Actress Renee Zellweger just celebrated her 55th birthday, which she doesn’t take for granted. Nearly three decades ago, the “Bridget Jones’ Diary” star once experienced a cancer scare that conjured up memories of her late grandmother who died from cancer. Since then, regular check-ups and cancer prevention have become a top priority.
“I pay attention; I do go get my check-ups,” Zelleweger previously told Self Magazine.

After learning the true nature of Zellweger’s lumps, she chose to have them removed.
“Get in there, stab away, get your little crunch bit or whatever you’re looking for, put it in the mail, and we’ll call it a day,” Zellweger described as she prepared for the procedure.
“My grandmother died from it, and two aunts were also diagnosed with it, but it was after a close friend’s diagnosis ten years ago that I saw how brutal breast cancer can be, how it can take over someone’s life, and yet they can fight it with dignity and survive it that’s inspirational,” she told Glamour.com.
Expert Resources on Breast Cancer Screening
- Millions of Women With Dense Breasts — A New Congressional Law — What You Need to Know
- 6 Common Excuses for Skipping a Mammogram That You Need to Stop Using!
- Mammograms Are Still the Best Tool for Detecting Breast Cancer — A Warning About Thermography
- I Have Dense Breasts. Do I Need a 3D Mammogram?
- New Guidelines Say Many Women Under 50 Can Skip Mammograms. That May Not Be The Best Advice
When to Screen for Breast Cancer
The medical community has a broad consensus that women have annual mammograms between the ages of 45 and 54. However, an independent panel of experts called the U.S. Preventive Services Task Force (USPSTF) is saying that women should now start getting mammograms every other year at the age of 40, suggesting that this lowered the age for breast cancer screening could save 19% more lives.
The American Cancer Society recommends yearly mammograms for women 55 and older. However, women in this age group who want added reassurance can still get annual mammograms.
WATCH: Mammograms are still the best tool for detecting breast cancer.
Women with a strong family history of breast cancer, a genetic mutation known to increase the risk of breast cancer, such as a BRCA gene mutation, or a medical history, including chest radiation therapy before the age of 30, are considered at higher risk for breast cancer.
Experiencing menstruation at an early age (before 12) or having dense breasts can also put you into a high-risk category. If you are at a higher risk for developing breast cancer, you should begin screening earlier.
Screening Options for Women with Dense Breasts
Women with dense breasts should get additional screening to supplement their mammograms. Dense breasts mean more fibroglandular tissue and less fatty breast tissue exists.
The dense tissue has a “masking effect on how well we can perceive cancer and find cancer on mammograms,” Dr. Cindy Ly, Chief of Breast Imaging and Vice Chair of Clinical Research and Faculty Affairs at the Stony Brook Renaissance School of Medicine, told SurvivorNet.
Glandular tissue within dense breasts appears white on mammograms, which can help mask potential cancer. The “frosted glass” effect from the glandular tissue can thus mask cancerous areas, especially developing ones. Undetected, these cancers can progress, growing large and advanced. They will then likely require more intensive treatments to cure or can become incurable altogether.
WATCH: What is 3D Mammography?
“Digital mammography, it turns out, significantly improves the quality of the mammogram…It’s 3D or tomosynthesis mammography,” Dr. Connie Lehman, a diagnostic radiologist specializing in breast cancer at Massachusetts General Hospital in Boston, explains.
“This allows us to find more cancers and to significantly reduce our false-positive rate. With digital mammography 3D tomosynthesis, we’re taking thin slices through that breast tissue, like slices of a loaf of bread. We can look at each slice independently rather than trying to see through the entire thickness of the entire loaf of bread. So those thin slices help us find things that were hidden in all the multiple layers,” Dr. Lehman adds.
Additional testing can be considered for dense breasts, depending on a woman’s personal history, preferences, and physician’s guidance. These tests include:
- 3-D Mammogram (Breast Tomosynthesis): This technology acquires breast imaging from multiple angles and digitally combines them into a 3D representation of the breast tissue. This allows physicians to see breast tissue architecture better, even in dense breasts. 3D mammograms are fast becoming the standard way of performing mammography.
- Breast Magnetic Resonance Imaging (MRI): An MRI machine uses magnets to create highly detailed, intricate images of the breast. These are mostly reserved for women with an extremely high breast cancer risk. Dense breasts alone may not be a valid reason to obtain a breast MRI. However, dense breasts in women with genetic mutations, like BRCA1 and BRCA2, or a strong family history of breast cancer could justify obtaining breast MRIs.
- Molecular Breast Imaging (MBI): MBI is a newer imaging technique that uses a radioactive tracer to detect breast cancer. It is beneficial for women with dense breasts. However, MBI is not as widely available as other screening methods.
The Food and Drug Administration (FDA) ruled that facilities offering mammograms must notify patients about their breast tissue density and recommend they speak with a doctor to determine if further screening is necessary. There will be “uniform guidance” on what language to use and what details to share with the patient to make the communication clear and understandable.
Help Coping With a Breast Cancer Diagnosis
If you are facing a breast cancer diagnosis, your emotions are likely to run high, which is completely normal. Psychiatrist Dr. Lori Plutchik says emotions are often fluid when coping with a diagnosis.
“The patient or person going through the stressful event should accept that emotions will be fluid. You may feel fine one day and then feel a massive wave of stress the next. It’s also important for those you look to for support, whether that’s a therapist, friends, and family, or both, to understand the fluidity of stress-related emotions,” Dr. Plutchik said.
WATCH: How to cope with complex and changing emotions.
If a stressful event affects how you think and feel, it may be time to seek mental health treatment. This could mean traditional talk therapy, medication, changing lifestyle habits (like exercise and diet), seeking a support group, or many other approaches.
Here are some helpful tips for women needing a little extra help coping with a breast cancer diagnosis.
- Let your family and close friends know and let them help. So many cancer survivors tell us they want and need support but are often too preoccupied to make specific requests. Urge those close to you to jump in with whatever practical help they can offer.
- Keep a journal. It can be highly cathartic to let those feelings loose on paper. Grab a pen and a lovely journal and chronicle your thoughts throughout the day.
- Join a cancer support group. Groups are available in nearly every community and offer opportunities to connect with others going through a similar journey. You’ll learn constructive insight from others who can tell you what to expect and how to stay strong on tough days.
- Consider seeing a therapist. Ask your doctor to refer you to a therapist so you can discuss your fears and concerns in a safe space. Often, vocalizing your thoughts and feelings rather than internalizing them can provide relief.
Questions for Your Doctor
If you have a breast cancer screening coming up or recently had one, you may have questions you want answered. SurvivorNet suggests the following questions to kickstart your conversation with your doctor.
- Do my mammogram results indicate I have breast cancer, or am I at higher risk?
- If I’m at higher risk, what are my treatment options?
- What side effects should I expect related to my treatment?
- How much will this diagnosis prevent me from working or fulfilling my daily activities?
- Will insurance cover my breast cancer screening, or are there other financial resources available?
Learn more about SurvivorNet's rigorous medical review process.

