Advances in Multiple Myeloma
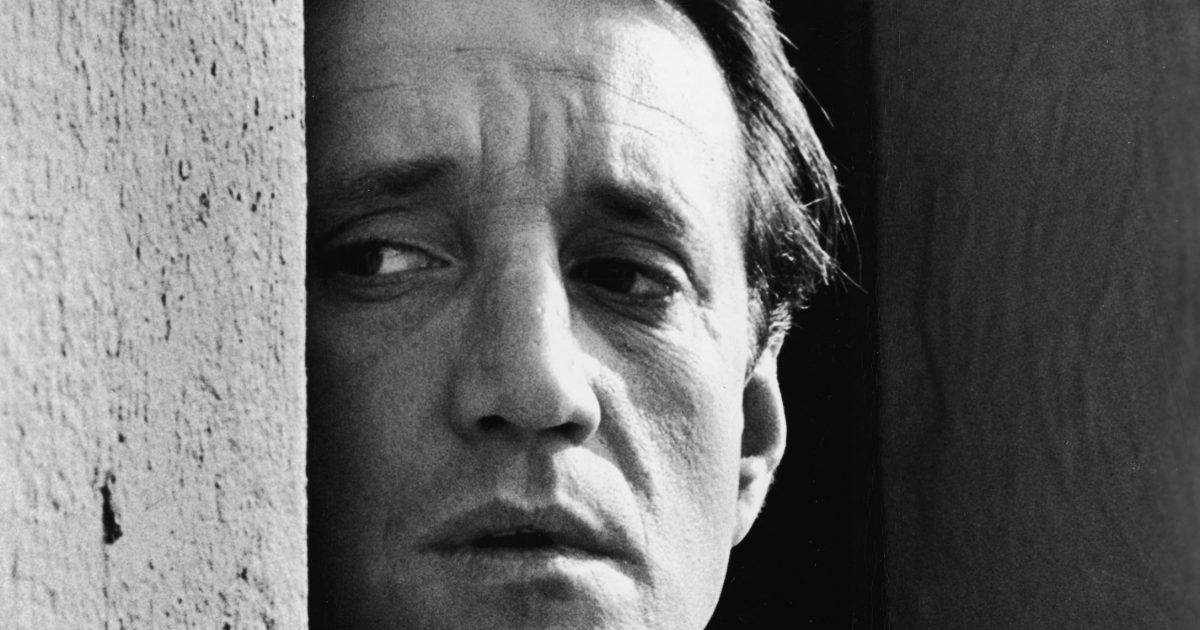
- Beloved “Jaws” police chief Roy Scheider died of complications from a staph infection in February 2008, after having battled multiple myeloma cancer for several years.
- Multiple myeloma is a cancer of the bone marrow that can lead to things like fatigue, bone fractures and kidney damage.
- There is, technically, no cure for multiple myeloma, but recent advances in medicine are hopeful.
- Doctors are studying the impact of four-drug regimens versus three drug regimens for induction therapy the first phase of multiple myeloma treatment.
- And CAR T-cell therapy is a treatment that genetically engineers a patient's own immune cells to attack cancer cells.
- BiTE (bispecific T-cell engager) is another form of treatment that’s being studied.
- Improvements in maintenance therapy the last stage of multiple myeloma treatment include Revlimid, “considered standard of care at this time,” according to one of our experts.
- In addition, the bispecific monoclonal antibody drug Tecvayli was recently FDA approved to treat adults with multiple myeloma that came back or did not get better after treatment with at least four other anticancer therapies.
Scheider notably portrayed the police chief of Steven Spielberg's 1975 breakthrough hit “Jaws” and uttered one of the most famous lines in movie history: “You’re gonna need a bigger boat.” In 2005, that line was voted No. 35 on the American Film Institute’s list of best quotes from U.S. movies.
Read MoreScheider died of complications from a staph infection in February 2008 at age 75, after having battled multiple myeloma for several years. He reportedly underwent a bone-marrow transplant for his cancer in 2005, but he stayed busy all the way up until his passing. The New York Times says he was even involved in a project to build a film studio in Florence, Italy, for a series about the history of the Renaissance at the time of his death.
Understanding Roy Scheider’s Type of Cancer: Multiple Myeloma
Multiple myeloma is a type of blood cancer that involves plasma cells a certain kind of mature white blood cell in the bone marrow that helps fight infection by making proteins that supports your immune systems fight against germs. In order to understand this disease, it's important to talk about the bone marrow.
What Is a Blood Cancer How Is It Different?
"The bone marrow is the factory that makes all of the cells that wind up in our bloodstream," Dr. Mikkael Sekeres, the chief of the Division of Hematology at the University of Miami Sylvester Comprehensive Cancer Center, previously told SurvivorNet.
The bone marrow makes red blood cells which bring oxygen to our tissues, white blood cells which fight infections and platelets which help stop bleeding. People with multiple myeloma have cancerous plasma cells, or myelomas, that grow uncontrollably in the bone marrow and crowd out healthy white blood cells which hinders the immune system's ability to fight off infection.
RELATED: For Father Of Four, 43, Soreness From New Orange Theory Gym Kick Turned Out To Be Cancer
Bone fractures can eventually form when the myelomas grow too large in the bone marrow. Kidney damage can also occur because the myelomas release abnormally high levels of antibodies into the bloodstream which eventually build up in the kidney since its unable to process the excess proteins.
Dr. Nina Shah, a hematologist-oncologist with University of California at San Francisco, spoke with SurvivorNet about some of the symptoms of multiple myeloma.
"It's very common for someone to say, 'You know, I've been feeling very tired," or 'You know, I notice I had a few more infections last winter than I remember,'" Dr. Shah said. "But at the first sign of something abnormal, it's important to then take that to the next step and say, 'OK, what am I missing? Is there something else maybe that could be causing this?' And that's often when we see a diagnosis of multiple myeloma."
Furthermore, bone problems like pain or weakness in the back, hips or skull are other symptoms to look out for with multiple myeloma.
There is, technically, no cure for multiple myeloma, but recent advances in medicine are hopeful especially with early diagnoses.
"This is still considered an incurable disease," Dr. Shah said. "But we want to make sure we make people understand that it's a disease that you can live with not necessarily have to die of."
Just in the 15 years since Schedier battled the disease, multiple myeloma treatments have come far. Doctors are working on and studying options that give patients more sustainable treatment plans, and there is now a standard of care that helps keep the disease under better control thereby helping people live longer.
Advances in Myeloma Treatment
Promising advancements for multiple myeloma treatment are being made in each phase of disease treatment. With induction therapy, for example, doctors are studying the impact of four-drug regimens versus three-drug regimens. Induction therapy is the first phase of treatment, with the goal of reducing the number of myeloma cells within your bone marrow to prepare for a stem cell transplant (if you're eligible).
According to Dr. Tareq Al Baghdadi, a medical oncologist and hematologist at St. Joe's Mercy Hospital in Ann Arbor, Michigan, the triple regimen of VRD is the "standard."
- Bortezomib (Velcade) a proteasome inhibitor
- Lenalidomide (Revlimid) an immunomodulatory drug
- Dexamethasone a steroid
Dr. Al Baghdadi says triplet regimens have been giving patients “deeper and longer responses,” but some doctors are adding a fourth drug the monoclonal antibody daratumumab (Darzalex) into the mix.
"With regards to induction therapy, three versus four drugs, there's early data now showing that you achieve deeper responses when when you use four drugs versus three drugs, but whether that's gonna lead to survival advantage remains to be seen and specifically which subgroup of patients will achieve that advantage," he said. "Is a four drug regimen preferable in high risk patient versus low risk patients or standard risk patients versus both? That's what the current clinical trials are assessing."
CAR T-cell therapy has also been coming onto the scene for multiple myeloma treatment. In general, CAR T-cell therapy or chimeric antigen receptor T-cell therapy is a treatment that genetically engineers a patient's own immune cells to attack cancer cells.
“We’re trying to incorporate CAR T-cell therapy sooner in the treatment protocol rather than wait until the patients has had multiple treatment for relapsed and refractory multiple myeloma,” Dr. Al Baghdadi said.
Similarly, allogeneic CAR T-cell therapy is where genetically engineered immune cells from another person, typically a donor who closely matches the recipient, are given to a patient. This eliminates the need to harvest and modify the patient’s own cells.
CAR T-cell therapy is considered to be a very promising new treatment option for multiple myeloma, but BiTE (bispecific T-cell engager) is also being studied. This form of treatment uses a patient’s own cells to fight cancer, but, in this case, the cells are given an antibody that attaches to both the cancer cell and your T-cells instead of being genetically modified. From there, BiTEs activate the immune cells to signal other cells to attack and destroy the cancer cells.
RELATED: CAR T-Cell Therapy and BiTE: Two New Approaches to Multiple Myeloma Treatment
"BiTEs are a different form of therapy that are more continuous in nature," Dr. James Hoffman, hematologist at the Sylvester Comprehensive Cancer Center at the University of Miami, told SurvivorNet. "They harness the patient's immune system using the BiTEs or the bio-specifics.
"Patients receive these medications on some sort of regular basis, for example, every two weeks. These are molecules that have two arms to them, one arm that grabs the myeloma and another arm that grabs the T-cell and it basically introduces the T-cell to the myeloma within the individual patient."
Because the antibody used to bond the cancer cell does not need to be tailored to each patient, unlike in CAR T-cell therapy, BiTE may be a more affordable and accessible option in the future.
Improvements in maintenance therapy are also being made. Maintenance therapy is the last stage of multiple myeloma treatment meant to keep the cancer under control after you've had other forms of treatment.
"With regards to maintenance therapy in multiple myeloma patients, this is mainly studied in patients who have had autologous stem cell transplantation, and there's been multiple clinical trials looking at different medications over the years," Dr. Al Baghdadi said. "And the one that showed the most benefit and considered standard of care at this time is Revlimid.
“This is especially the case in standard-risk patients who can go on two years of Revlimid, and, with that, achieve an improvement in disease control and survival."
The Future of Multiple Myeloma Treatment
Revlimid is the brand name for the immunomodulatory drug lenalidomide. An immunomodulatory drug is used to modify a person's immune system response. Revlimid is also commonly seen as part of induction therapy, and it is not the only maintenance therapy drug option. For high-risk multiple myeloma patients, for example, Dr. Al Baghdadi has seen that another drug can be a suitable option.
RELATED: How Are Patients Monitored After Multiple Myeloma Treatment?
"The quality of the data in [higher-risk] patients is not as good as the data with Revlimid, but data in high risk patients also show that a drug like Velcade can improve disease control and survival," he said. "So you'll see some patients going on maintenance with Velcade and occasionally with both drugs, Velcade and Revlimid."
In addition, Dr. Al Baghdadi said researchers are looking into adding more drugs in the maintenance therapy stage of multiple myeloma treatment.
“For example, we’re looking at adding a drug called Ninlaro to patients on Revlimid, especially if they don’t achieve MRD negativity while on revlimid,” he explained. “We’re also looking at other antibodies like daratumumab (sold under the brand name Darzalex) also during maintenance.”
Which Multiple Myeloma Drugs For Maintenance Therapy: Are There Options?
Darzalex is a type of targeted monoclonal antibody. Monoclonal antibodies are drugs that target specific proteins on cancer cells. In the case of Darzalex, the CD 38 protein in the target.
But as recently as October 25, 2022, Tecvayli was FDA approved to treat adults with multiple myeloma that came back or did not get better after treatment with at least four other anticancer therapies. This drug is a type of bispecific monoclonal antibody that binds to a protein called CD3, which is found on T cells, and a protein called BCMA, which is found on myeloma cells and some B cells.
Bispecific antibodies, in general, are a type of monoclonal antibody that targets two different types of molecules, or antigens. They are engineered to bind to myeloma cells and either kill them or flag them for destruction by your immune system. This type of treatment is effective in fighting cancer by stimulating an innate immune response against specific tumor-associated antigens.
"There are probably 20 or 30 of these antibodies in development for multiple myeloma, as we speak," Dr. C. Ola Landgren, the leader of the Experimental Therapeutics Program and leader of Myeloma Service at Sylvester Comprehensive Cancer Center, said in an interview with SurvivorNet prior to the Tecvayli approval. "Many of these drugs are just amazing."
It's important to note there isn't one clear answer when it comes to multiple myeloma treatment. Make sure you have a comprehensive conversation with your doctors to decide what treatment path is best for you and consider all of your options.
Learn more about SurvivorNet's rigorous medical review process.