Removing The Stgma From Male Breast Cancer
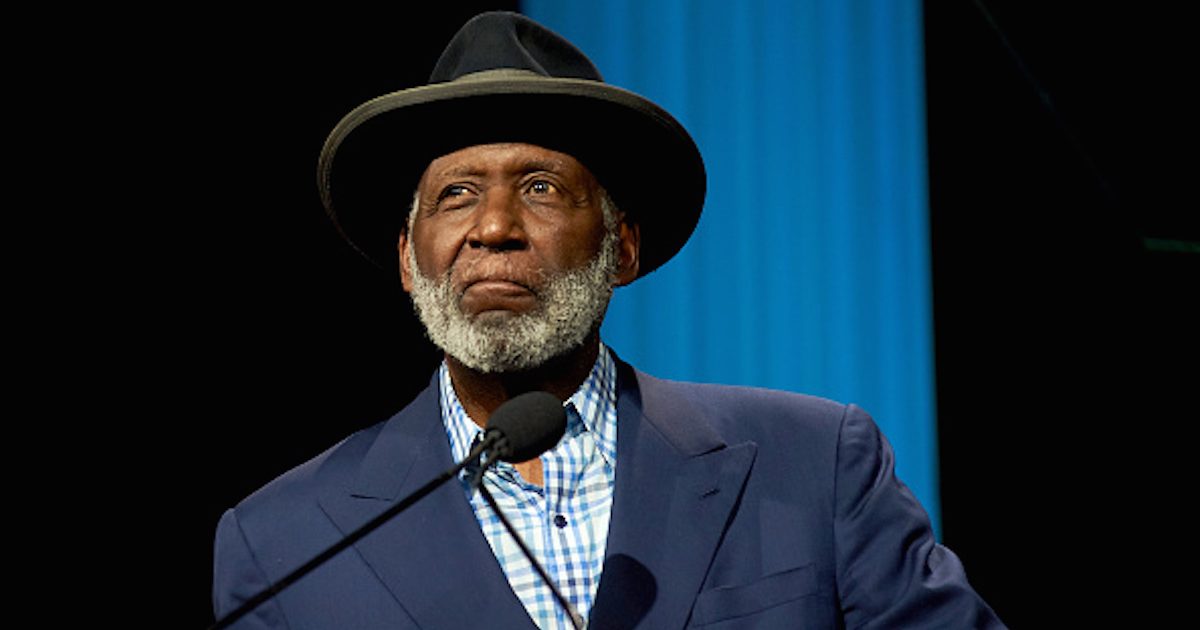
- “Shaft” action hero Richard Roundtree, 80, was shocked and embarrassed when he was diagnosed with male breast cancer back in 1993.
- He underwent a double mastectomy and chemotherapy to beat the disease.
- Treatment for male breast cancer is largely the same as female breast cancer, say experts. While men do have some special considerations, treatment options depend greatly on a variety of factors, including the size of the tumor and how far the cancer cells have spread, as well as biological and genetic factors that may be powering your cancer.
- Treatment options may include surgery, chemotherapy, hormone therapy, radiation therapy and targeted therapy.
- Two-time breast cancer survivor Marc Futterweit knows how debilitating the shame can be, but overcoming it and getting your symptoms checked can help save your life.
What has changed in breast cancer treatment in the three decades since his diagnosis?
Richard Roundtree’s Surprising Breast Cancer Diagnosis
Read More
This attention to changes in his body was crucial. One doctor told USAToday at the time that man may be less likely to report changes in their breasts, leading to lower survival rates.
“Three days later I received the we-need-to-talk call that immediately sent up red flags for me like crazy. When he sat me down and told me I had cancer so many things went through my mind but the first was, "Wait, did he just say I had breast cancer? That word scared the bejeezus out of me!” he explained. “I couldn't relate and I thought he was questioning my manhood because women die from this, not men. How could I possibly have that? But I soon learned that this disease is not gender-based.”
Roundtree continued, “Ironically, my only trepidation was sharing my condition with anyone in Hollywood because the industry doesn't like sick people. I was never concerned about telling any of my male friends, but the industry, yes, so I never let on and I never told anyone until I was cancer-free and a five-year survivor.”
The actor, who is starring in the upcoming comedy “Moving On” with Jane Fonda, has since been urging others to “get more than one diagnosis.”
The father of five had experienced some shame around his diagnosis, saying that didn’t tell anyone in the entertanment industry. And he has admitted that he still has some of those insecurities after beating the disease.
He told Extra TV in 2019, “I’m not a real beach person to begin with, but taking off my top is an issue. I still look in the mirror as I pass the mirror in the morning out of the shower (points to chest) and there’s no feeling under the arm I still have issues."
However, Roundtree is thankful for going public with his cancer journey as he’s now become an advocate for the disease and has worked with the Susan G. Komen Breast Cancer Foundation.
"Coming out of the closet about my breast cancer episode, that was an eye-opener for me because I really got to experience the fact that men are so cavalier about their health issues and want to sweep it under the rug,” he told Extra. “So I came out about it and the response was incredible."
What Has Changed For Breast Cancer In 30 Years?
Since Roundtree’s diagnosis, there has been a new classification of some advanced breast cancers called "HER2-low,” which means that women previously classified as HER2-negative could qualify for certain treatments.
Breast cancer cells with higher than normal levels of HER2 are called HER2-positive, found in 15-20% or all breast tumors. While they tend to grow faster, they are much more likely to respond to treatment with drugs that target the HER2 protein.
HER2-low cancers do not meet the threshold for HER2 positive tumors, but they still have a minimal amount of HER2 expression. So with the new grouping, HER2-low patients that may have previously been classified as HER2-negative may have the ability to take advantage of life-changing treatments like Enhertu, which can extend overall survival rates.
Understanding Male Breast Cancer
The lifetime risk of getting breast cancer is about 1 in 833 for men. In addition, the American Cancer Society estimates that about 2,800 new cases of invasive breast cancer will be diagnosed in men in the United States in 2023.
There are several risk factors that can increase a man's chance of developing the disease, just like in the case of female breast cancer. If you're a man with any, all or some of the following risk factors, vigilance is key.
Possible Risk Factors for Male Breast Cancer:
- Age. Breast cancer risk increases with age, and most cancers are found in patients over 50. The average age of a man diagnosed with breast cancer is 72.
- Family history. Men with close blood relatives who have had breast cancer are at higher risk for the disease.
- Genetic mutations. Patients may inherit gene defects that make them more susceptible to breast cancer. Men with a mutation in the BRCA2 gene have a 6 percent lifetime risk of developing breast cancer, and men with a mutation in the BRCA1 gene have a 1 percent lifetime risk. These gene mutations are most commonly found in families with strong histories of breast or ovarian cancer, but they have also been found in male breast cancer patients without a family history.
- Klinefelter syndrome. Men with Klinefelter syndrome are born with at least one extra X chromosome which may increase a man's breast cancer risk by producing high levels of estrogen (a hormone responsible for female sex characteristics) and low levels of androgens (hormones responsible for male sex characteristics). This condition affects about 1 in 1,000 men, and can raise the risk of breast cancer by 20 60 times that of the general population.
- Hormone therapy. Men who have been treated with drugs containing estrogen are at a greater breast cancer risk. These drugs were once used to treat prostate cancer, and they are still used in sex reassignment processes.
- Conditions affecting the testicles. Testicle injuries, swelling or removal surgery can increase a man's risk for the disease by disrupting normal hormone levels.
- Liver disease. Diseases that impede the liver (like cirrhosis) may raise men's estrogen production and lower their androgen levels, therefore, increasing breast cancer risk.
- Alcohol. Heavy drinking is known to raise the risk of breast cancer (which may be related to alcohol's effect on the liver).
- Radiation therapy. Men who have received radiation therapy to their chests (for conditions like lymphoma) have a higher risk of developing breast cancer.
- Obesity. Fat cells can transform androgens into estrogens, boosting the possibility of an overweight man developing breast cancer.
If any of the above risk factors applies to you, consult your doctor and feel free to ask questions. While it's true that men can work to lower their breast cancer risk by exercising and maintaining a healthy bodyweight, the most important element of effective cancer treatment is an early diagnosis.
Symptoms of Male Breast Cancer Can Include:
- A lump developed in the breast (usually painless), or a thickening in the breast tissue
- Nipple pain
- An inverted nipple
- Discharge from the nipple, which may be clear or bloody (this was Mathew Knowles' first symptom)
- Changes to the color or texture of the nipple and areola
- Changes to the color or texture of skin on the chest
- Enlarged lymph nodes under the arm
If You Feel Something, Say Something Men Ignore Symptoms Too Often
Treatment for male breast cancer is largely the same as female breast cancer. A person's options depend greatly on a variety of factors, including the size of the tumor and how far the cancer cells have spread, but possibilities include surgery, chemotherapy, hormone therapy, radiation therapy and targeted therapy.
Treating Breast Cancer
Doctors treating breast cancer look for markers on your particular cancer to help decide what course of treatment is best for you. That's because cancer cells may have what are called receptors that help identify the unique features of the cancer.
The three main receptors are the estrogen receptor, the progesterone receptor, and the HER2 receptor. The estrogen and progesterone receptors go together because they are fueled by hormones. Think of the cancer cell as having little hands on the outside of the cell which grab hold of proteins that help it grow. These proteins are sometimes called "ligands."
An example of a type of ligand that can stimulate a cancer cell is the hormone estrogen. An estrogen receptor-positive breast cancer will be stimulated by estrogen to grow. In this instance, your doctor may offer you treatment to specifically target the estrogen receptor.
Another important receptor to test for is the HER2 receptor. For HER2 positive breast cancers, therapies that uniquely target the HER2 receptor are essential to treating the disease.
What Happens During a Double Mastectomy?
A double mastectomy, like Roundhouse underwent, is a procedure in which both breasts are removed to get rid of cancer.
“Most men with breast cancer will undergo a mastectomy since men have a small amount of breast tissue,” the American Cancer Society explains.
The procedure may also be performed as a preventative measure for women who are at a very high risk of developing breast cancer, such as those with the BRCA1 or BRCA2 gene mutations.
The procedure typically only takes a few hours, but may take longer depending on what type of reconstruction a woman has opted to get. Some women decide to have their breasts reconstructed and have implants put in right after the mastectomy, while others don't have reconstruction at all.
"A double mastectomy typically takes about two hours for the cancer part of the operation, the removing of the tissue," Dr. Elisa Port, Chief of Breast Surgery at Mount Sinai Health System, tells SurvivorNet. "The real length, the total length of the surgery, can often depend on what type of reconstruction [a patient] has."
Learning About Double Mastectomy
There Is Nothing To Be Ashamed Of With Male Breast Cancer
Marc Futterweit is a two-time breast cancer survivor and he knows first-hand that the shame that comes with a diagnosis of male breast cancer can be quite debilitating. The urge to just ignore the symptoms may sway you from getting screened. But Marc has become an advocate for the disease, and is now dedicated to halting that way of thinking.
"Men are basically standing in the shadows," Marc says. "They're ashamed or embarrassed … this is a woman's disease. [But] why can't men get breast cancer?"
A lot of people assume men can't even get breast cancer because they don't have breasts, but that's not the case. The American Cancer Society estimates that about 2,550 men will be diagnosed with breast cancer every year in the United States, and 480 men will die from it. It's much less common in men than it is in women (the lifetime risk of a man getting breast cancer is about 1 in 833), but surveillance and screening is still important.
That's why Marc's philosophy is "if you feel something, say something." He detected his own cancer when he felt an odd lump on his chest during a shower. He admits, he was baffled when his doctor suggested he get a mammogram, but in reality, it probably saved his life. "The problem with men is that they wait, and they think things are going to go away," Marc says. "Once they're diagnosed, sometimes it's too late."
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.