Reclaiming Life After Cancer
- Rock icon Ann Wilson of Heart is disclosing more about her health fight as the “Barracuda” singer has finished chemotherapy treatment, which she says is “no joke,” and empathizes with people experiencing the “mental torture” of waiting for test results — thankfully, she “got the good kind” and is ready to resume her rock ‘n’ roll tour with her sister Nancy Wilson.
- The legendary sisters, who formed Heart back in 1973, had a full tour lined up from July to December of this year, but in light of Ann’s cancer diagnosis, shared to fans in July, the band had to postpone to 2025.
- During — or at the tail end — of a patient’s chemotherapy treatment, they will often get follow-up scans or other tests to check the status of their disease, which has either been eradicated, managed/reduced, or sometimes it unfortunately has progressed. The waiting game is often the most stressful.
- Scan anxiety, or “Scanxiety,” is the uneasiness cancer survivors experience in anticipation of scans that could show a relapse or recurrence in their disease. Staying busy with friends and family or doing things you love to distract yourself during this tumultuous waiting period can be helpful to make the time pass by more quickly. No matter what the results show, trying to incorporate the things in your life that bring you the most joy will always help to continue living your life
The musician, 74, known for her husky voice and ability to wail out the high notes, gave an update via voiceover in a reel with scrolling text next to a sultry photo with her signature shag and smoky eyes.
Read More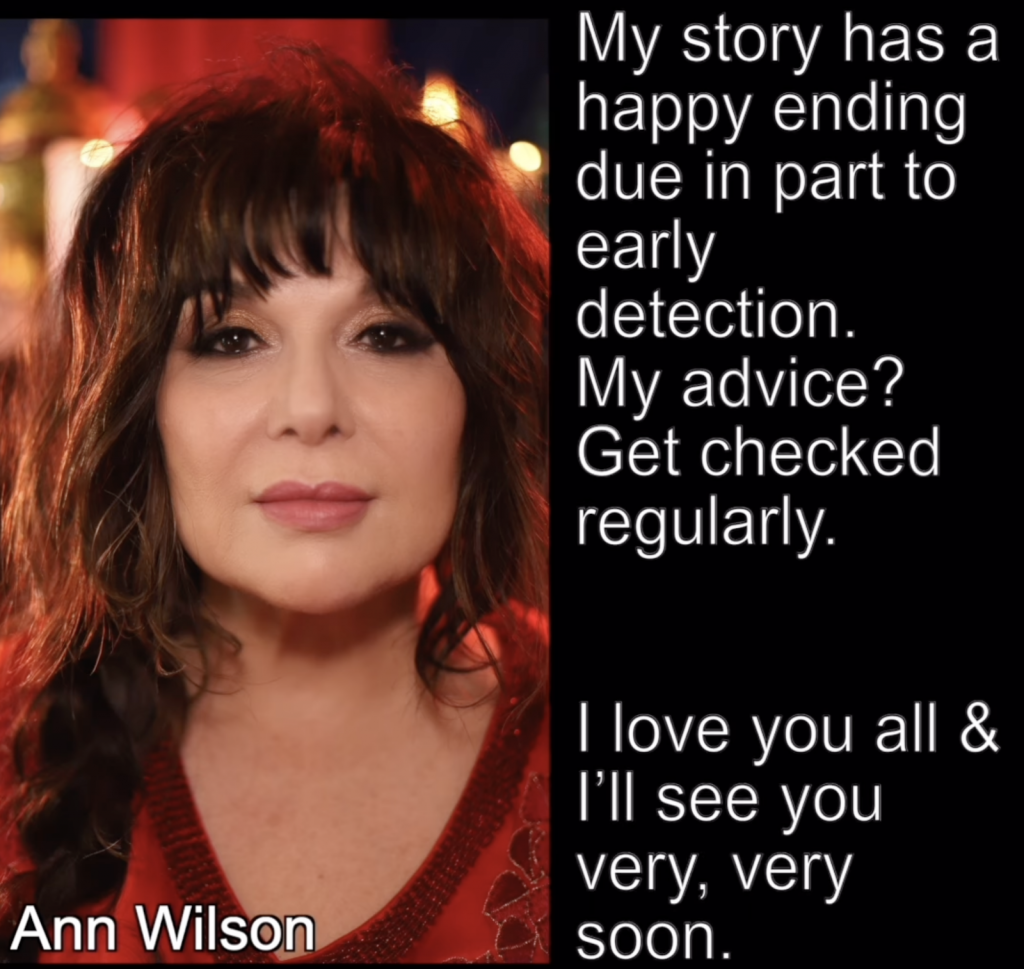
“There’s maintenance going forward,” Ann continued in her update, “but I’m told the side effects are much less severe. The worst is over and I’m thankful for the efficacy of this poison — but it’s more than welcome to get the f— out of my body now.”

Noting that she is “immensely grateful” for all the support she’s received since making her first announcement, she urged regular check-ups. “My story has a happy ending due in part to early detection.”
“My advice? Get checked regularly. I love you all and I’ll see you very, very soon. There’s much to celebrate.”
View this post on Instagram
Ann Wilson’s Cancer Diagnosis
Ann first announced her cancer diagnosis and treatment plan in July, which is also when she delivered the news of postponing her tour.
“Dear friends,” Ann began in a letter posted to her Instagram account. “I recently underwent an operation to remove something that, as it turns out, was cancerous. The operation was successful & I’m feeling great but my doctors are now advising me to undergo a course of preventative chemotherapy & I’ve decided to do it.”
“And so my doctors are instructing me to take the rest of the year away from the stage in order to fully recover.”
“To the ticket buyers,” she continued, “I really do wish we could do these gigs. Please know that I absolutely plan to be back on stage in 2025. My team is getting those details sorted & we’ll let you know the plan as soon as we can.”
“I’m a little disappointed, but that means nothing to me. What means everything to me is that you’re healthy,” one fan wrote on Ann’s post. “Concerts and this and that can definitely wait. Take care of yourself. We’re all right behind you no matter what. Sending love and support.”
The Reuniting of the Legendary Sisters of Rock
Ann and Nancy Wilson launched the first female-fronted mega-rock band with Heart in 1973. They released top hits such as “Crazy on You” (1975), “Magic Man” (1976), and later, “Alone” (1987), which are still as popular as ever with younger generations today.
Up until they joined forces again, Nancy had been on a solo tour with her band Trip Sitter.

In October, Nancy and Ann reunited for the first time onstage since 2019, as a complete surprise to fans who went wild when Nancy took the stage at Luther Burbank Center for the Arts in Santa Rosa, Calif., for a rendition of one of Heart’s other top early hits, “Barracuda” (1977).
“Ladies and gentlemen, we have the answer to a question with us tonight,” Ann said. “A very, very good friend, more than a friend. Let’s bring her out. Come on.”
Later on, the legendary siblings gave press interviews together, even addressing their private issues, and much to fans’ delight, announced the tour.
Ann’s manager Dave Frey, in a statement with the Washington Post, summed it up perfectly. “Nancy singing with Ann is like Keith [Richards] singing with Mick [Jagger],” Frey said, comparing their energy to the fellow legendary Rolling Stones duo. “It’s the secret sauce. I didn’t realize that until I heard it.”
Therefore, the added pressure of Ann’s health news for her as an artist is tough to think about, but health must always come first — and thankfully her dedicated fans support that. After all, she has made it clear that this is just a postponing of dates, not a cancellation. And so far, it looks like it’s all working out.
Understanding Chemotherapy Treatment
Chemotherapy uses strong drugs to kill cancer all over the body. You may get this treatment to shrink a tumor before surgery, afterward to get rid of any remaining cancer cells or on its own if you can’t have surgery.
Whether or not to have chemotherapy can also be a choice, depending on a woman’s age, type of cancer, and stage.
Ann has not yet shared further details of the type of cancer she has been facing. Chemotherapy affects everyone differently, so there are no definite side effects you can count on.
Below are some of the more common side effects that can affect patients during and after treatment. And while it is important to note that we’ve come a long with the management of these side effects, they can still have a great impact on people during their cancer battle.
Nausea
“One of the things that patients worry most about is nausea with chemotherapy,” Dr. Michael Ulm, gynecologic oncologist at West Cancer Center, said during a previous interview with SurvivorNet. "Everybody remembers what their parents went through or what their aunts and uncles went through probably 15 or 20 years ago.”
Even though people can still anticipate nausea, Dr. Ulm said your nausea shouldn’t be as bad as you’re imagining with today’s arsenal of effective treatments to combat the side effect with medications you can even take at home.
“I tell my patients, with modern medicine and modern antiemetics that you should never have severe nausea and you should never throw up,” Dr. Ulm said.
Hair Loss or Thinning
Many chemotherapies can cause hair loss or thinning.
Hair loss typically begins about three to four weeks after patients begin chemotherapy and continues throughout treatment. Patients can expect regrowth around four to six weeks after they complete treatment, but some patients may experience some changes to hair color and texture when it begins growing back.
The hair loss associated with chemotherapy is temporary, but this can be an incredibly distressing side effect for some. It is important to speak with your doctor about any personal issues that may be caused by treatment side effects, including the loss or thinning of your hair.
To help patients cope with hair loss, a doctor or nurse may be able to recommend a local wig-maker or other resources that can help slow down the process.
Heart Problems
Cardiotoxicity, or problems in the heart and vascular (circulation) system, can be a side effect of chemotherapy.
While uncommon, cardiovascular disease is the second leading cause of death among breast cancer survivors, behind only secondary malignancies due, in part, to the damage some cancer therapies can cause to the heart.
Certain Chemotherapy Treatments Are Linked to Higher Risk of Heart Problems
“From chemotherapy, high doses of anthracyclines, in particular, have been the prototype of cancer therapies that lead to cardiotoxicity,” Dr. Emanuel Finet, a transplant cardiologist at Cleveland Clinic Cancer Center, previously told SurvivorNet.
Cancer patients at a high risk for heart problems can be older, younger with more aggressive chemotherapy, obese, smokers or dealing with pre-existing cardiovascular disease.
Blood-Forming Cell Damage
Chemotherapy drugs can damage all three types of blood-forming cells: red blood cells, platelets and white blood cells. This in turn can lead to various issues like anemia (low red blood cell count), thrombocytopenia (low blood platelet account) or neutropenia (low number of a type of white blood cell called neutrophil).
“One of the things that’s changed in the coronavirus days is that now we’re giving everybody this drug called Neupogen or Neulasta, and it helps boost your white (blood cell) count,” Dr. Ulm recommended as a way to help your body fight infections.
Fatigue
Fatigue is another possible symptom that has the potential to worsen as chemotherapy cycles add up. If chemotherapy left you with anemia, you can try treating that ease exhaustion. But rest breaks, frequent exercise and getting plenty of sleep at night can also help fight fatigue.
In an earlier interview, Dr. Zachary Reese, a medical oncologist at Intermountain Healthcare, spoke with SurvivorNet about what chemotherapy-related fatigue is like.
“What I typically tell patients is that (chemotherapy) is a bit of a roller coaster ride,” he said. “You’re going to feel tired about a week into treatment, and that’s when you’ll hit bottom. And then you’ll start to come back up again just in time to do it all over. … You’ll feel a little more tired the second time around than you did the first, and it will last a day longer.”
Nerve Damage
Nerve damage, or neuropathy, can leave you with symptoms like “pins-and-needles,” pain, burning, numbness, weakness or trouble detecting heat and cold.
These symptoms might worsen as chemotherapy treatments progress, but there are ways to combat them. Steroids, numbing patches or cream, antidepressant medicine, anti-seizure medication physical therapy, relaxation techniques, acupuncture or dosage adjustments may help with these symptoms.
And while the symptoms of nerve damage might go away once you finish treatment, there can be lasting effects that require ongoing treatments.
Feelings of Anxiety While Waiting for Test Results
During — or at the tail end — of a patient’s chemotherapy treatment, they will often get follow-up scans or other tests to check the status of their disease, which has either been eradicated, managed/reduced, or sometimes it unfortunately has progressed.
Scan anxiety, or “Scanxiety,” is the uneasiness cancer survivors experience in anticipation of scans that could show a relapse or recurrence in their disease.
Psychiatrist Dr. Samantha Boardman, in a previous interview with SurvivorNet, offered practical tips on how to manage scanxiety. Here are her two top recommendations: Confront uncertainty and seek out the experience of flow.
“We know that uncertainty is an unbelievably uncomfortable place to be psychologically,” said Dr. Boardman. In fact, according to Dr. Boardman, studies have shown that people would often rather receive an electric shock than have to wait long periods of time to get information. “We’ll go to many lengths to try to get information at all costs,” she said.
Confronting uncertainty
To confront uncertainty, Dr. Boardman likes to encourage a simple exercise that starts with drawing four columns on a piece of paper. “I’ll ask patients to write down ‘what I don’t know, what I do know, what I can’t control, and what I can control,'” she said. From there, “a helpful way to dial down their anxiety” involves “trying to move as many items as possible into what they do know and what they can control.”
Visually mapping this process out on a piece of paper can also make patients feel more in-control of their circumstances. By taking the anxieties bouncing around in a person’s brain and putting them down in writing, patients are encouraged to feel like they have power over the challenges they’re up against.
SurvivorNetTV Presents: ‘Radical Age’ A Story of Seniors Defying Expectations
Seeking out the experience of flow
A second strategy that Dr. Boardman endorses is seeking out the experience of flow. “Scan anxiety is unbelievably stressful,” said Dr. Boardman. “And probably one of the best antidotes that I think psychology can offer patients is to experience flow.” Dr. Boardman defines flow as “that experience when you are so lost in an activity that you lose a sense of time.”
Not sure what that feels like?
“Probably the easiest way to think about it is an athlete or an artist when they are so embroiled in what they’re doing, that hours pass,” Dr. Boardman explained. She encourages patients to “embrace a hobby, something that we just do because we love doing it.” Finding flow can look different for everybody. “It might be baking. It might be gardening. It might be even doing some housework,” Dr. Boardman added.
The goal is for patients to find an activity that they can be so immersed in that they’re not thinking of anything else. “We know there’s data that shows that flow is a very good antidote for dealing with that anxiety and uncertainty,” said Dr. Boardman, “And especially, I think, patients can apply that to waiting for their scan results.”
Again, finding things that bring you joy every day can help distract from this tumultuous waiting period, and while it may not end with a North American tour, you can find ways to tap back into the activities that most bring you to life.
Learn more about SurvivorNet's rigorous medical review process.

