Understanding Glioblastoma
- Glioblastoma (GBM) is the most aggressive primary brain tumor.
- There is hope for patients through new clinical trials, including one using the modified poliovirus.
- Patients diagnosed with GBM may consider care at a top institution and enroll in a clinical trial.
"You are not dead just because you’re diagnosed with a glioblastoma.”
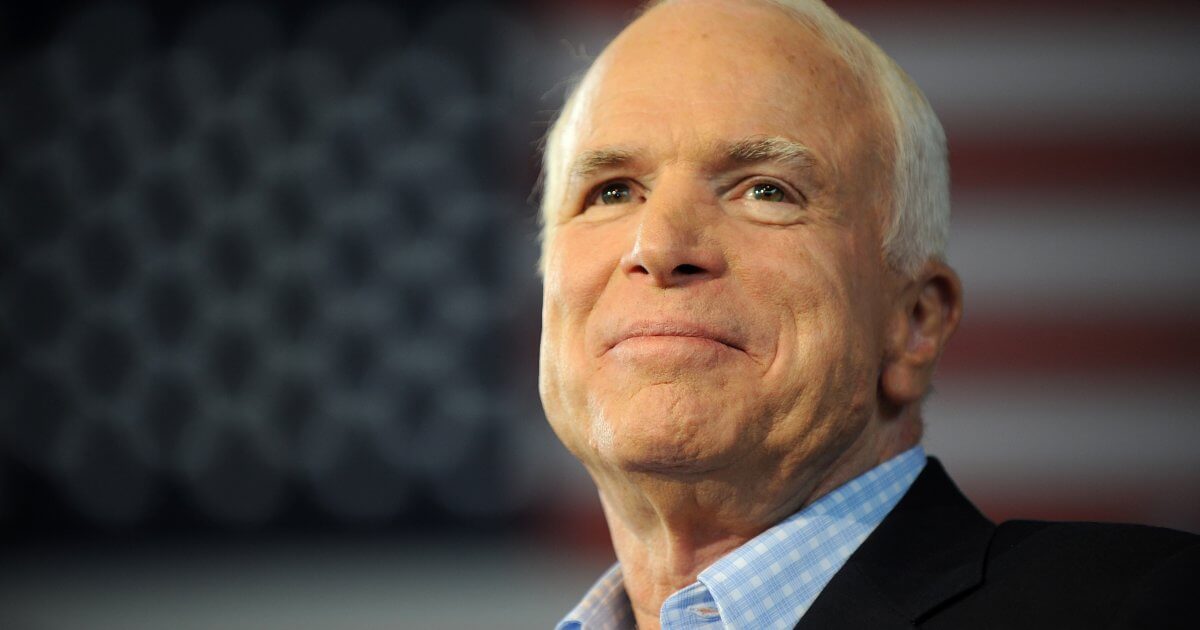
Glioblastoma, also called GBM, is the most aggressive brain tumor in adults. This is the type of cancer that John McCain and Ted Kennedy both had. Although rare, this tumor can divide rapidly and grow quickly. Despite the very best treatment options, outcomes are still modest, at best. Patients with GBM often have symptoms such as headaches, nausea, vomiting, and sensory changes such as issues with balance or walking. Sometimes GBM can also cause seizures and other neurological defects. Many of the symptoms a GBM may cause often improve following treatment.
New Hope for Those With Glioblastoma
Read MoreClinical Trials Offer Hope for the Future
While outcomes for patients with GBM are poor, clinical trials and future treatments offer some hope. Dr. Friedman and his colleagues at Duke University are investigating a new therapy that combines the modified poliovirus and immunotherapy. "The modified poliovirus is used to treat this tumor, by injecting it directly into the tumor, through a catheter. It is designed to lyse the tumor and cause the tumor cells to basically break up," he tells SurvivorNet. The goal is that the modified poliovirus will then trigger the body's own immune system to attack and fight the cancer cells. Because the poliovirus is injected only into the tumor, the researchers hope the body's natural immune cells will only attack and kill the cancer cells and not affect the normal, healthy brain tissue.When discussing the success of the poliovirus study, Dr. Friedman tells SurvivorNet, "It has helped a large number of patients, but not enough. We have a prolonged survival curve of about 18% going out many, many years in our initial trial. We don’t want to have 18%, 15%, 20% of people who are long-term survivors. We want them to be at a much higher number."
"I think that the modified poliovirus is going to be a game changer in glioblastoma, but I should also say that its reach is now extending into melanoma soon to bladder cancer."
Dr. Friedman and his colleagues are now taking this a step further by combining this treatment with a type of immunotherapy, called a checkpoint inhibitor. Specifically, the Duke team is using a drug called pembrolizumab (Keytruda) and is coupling it with the modified poliovirus. By combining these therapies the study team hopes the GBM patient's own immune system will be better equipped to attack and kill the cancer cells. While this is exciting, and certainly a point of hope for patients with GBM, this combination therapy needs to be tested in a clinical trial setting before it can be used to treat all patients with GBM. Currently, the researchers are working toward a clinical trial using the modified poliovirus with pembrolizumab for patients with recurrent GBM.
What is also exciting is that Dr. Friedman and his team think this combination of therapy may be successful in treating more than just GBM. "I think that the modified polio virus is going to be a game changer in glioblastoma, but I should also say that its reach is now extending into melanoma soon to bladder cancer," Dr. Friedman tells SurvivorNet.
While clinical trials such as the one above offer new hope, for patients who are not able to go on clinical trials, it's also important to understand the standard of care.
Understanding the Standard of Care for GBM
The standard of care treatment for a GBM patient usually consists of a surgical resection followed by radiation therapy and chemotherapy.
A neurosurgeon will try to take out as much of the tumor as possible without causing any damage to critical brain structures. Depending on where the patient's tumor is located, sometimes the surgeon can remove the entire tumor, while in other situations the surgeon is only able to remove a portion of the tumor. The goal, in both cases, is to get as much as possible in the safest way. After surgery, patients are given time to heal and regain their strength; usually during four to six weeks of recovery.
The next step is to start radiation therapy and chemotherapy. Most patients who need radiation therapy will have external beam radiation therapy, which is usually given every day (Monday – Friday) for six weeks, for a total of 30 treatments. Chemotherapy consists of a drug called temozolomide (also called Temodar) that is given daily with radiation. Unlike other chemotherapies, Temodar is a pill that is taken daily and does not require an IV or port placement. After radiation, patients will get additional chemotherapy using Temodar for 6 months or more depending on how they tolerate the medication.
Related: Fighting Brain Cancer With Electric Fields What is Optune?
Some physicians may also use a device called Optune, which goes on a patient's head. Several electrodes are attached to the patient's scalp to deliver an alternating electrical current. While patients do not feel this current, the Optune device has been shown to improve survival and slow tumor growth. However, it's not for everyone. Patients who use Optune will need to shave their heads and wear the device for most of the day, so it's important to discuss with your doctor about whether or not it's a good fit for you.
Although these treatments can help improve symptoms and slow tumor growth, a GBM tumor is so aggressive that it typically grows back after several months. Another standard of care option is to enroll in a clinical trial.
Learn more about SurvivorNet's rigorous medical review process.