Von Hippel-Lindau (VHL) is a rare genetic disease that is characterized by the formation of tumors or cysts affecting several organ systems. By the age of 65, 97% of people who have a VHL gene mutation will present with symptoms in up to ten parts of the body. The tumors that arise can be either non-cancerous (benign) or cancerous (malignant), with the most common tumor that presents in VHL being hemangioblastomas.
Von Hippel- Lindau Disease
VHL is an inherited genetic disease affecting 1 in 36,000 people, and 20% of cases are reported as de novo cases (first-in-family). There is a 50% chance that the gene alteration of VHL can be passed down to offspring if present in one parent. VHL disease is caused by an alteration (deletion or mutation) of the VHL gene, which is found on chromosome 3. This gene alteration can cause multiple types of tumors and cysts to manifest in different parts of the body. Unfortunately, if you have VHL, there is no precise way to predict where the tumors and cysts will grow; therefore, regular screening is very important. The mean age that symptoms start occurring in those with VHL is 26 years old, with 97% of people with a VHL gene mutation presenting with symptoms by the age of 65.
Where are Von Hippel-Lindau Disease and Tumors Mostly Found
Read MoreTumors involving the central nervous system (CNS):
Hemangioblasts are the most common symptom of VHL and are slow-growing benign tumors that arise in the retina, brain, and spinal cord. These tumors are made of newly formed blood vessels. In some cases, hemangioblasts in the spinal cord and brain may be confined within a cyst. The cysts or the hemangioblasts may cause additional symptoms such as headaches, weakness of the arms or legs, and balance problems when they put pressure on the brain or nerve tissue.Retinal Hemangioblasts, can cause vision loss if there is fluid or blood leakage from the tumor or if there is increased pressure from the tumor pushing on the tissue behind the eye. Retinal hemangioblasts can affect both the right and left sides of the body.
Endolymphatic Sac tumors (noncancerous tumors in the inner ear) occur in about 10% of people. Symptoms may include, sudden or gradual hearing loss, tinnitus (ringing of the ears), facial weakness, vertigo, the feeling of fullness in the ear, and dizziness.
Tumors involving the soft internal organs (Visceral) of the body
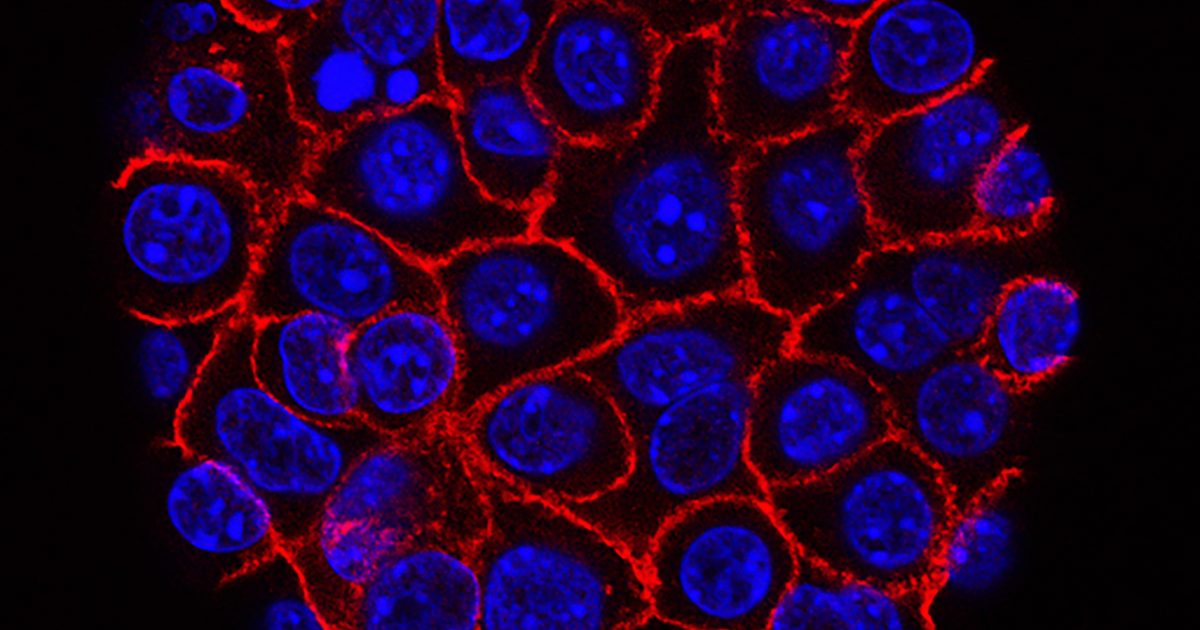
Renal cell carcinomas (kidney tumors) are cancerous (malignant) tumors that originate in the epithelium of the proximal convoluted renal tubule. Symptoms may include reduced kidney function, fever, fatigue, decreased appetite, blood in the urine, and back pain. These tumors will start to metastasize (spread) at approximately 3 cm in size if they are not removed.
Kidney cysts are noncancerous (benign) growths in the kidney that may present with high blood pressure, abdominal pain, and blood in the urine.
Phaeochromocytomas are cancerous (malignant) tumors of the adrenal gland, with symptoms consisting of nausea, heart palpitations, rapid pulse, headaches, anxiety, and clammy skin.
Epididymal Cystadenomas are noncancerous tumors that grow in the head of the epididymis. They can obstruct spermatic cords and efferent ductules. They usually do not present with symptoms.
Neuroendocrine tumors (PNET) are tumors that arise from within the islet cells (hormone-producing cells) of the pancreas. Symptoms include; jaundice (yellowing to the eyes and skin), vomiting, light color stool, dark urine, pain in the abdominal and back area, fatigue and tiredness, and unexplained weight loss.
VHL can be classified according to the tumors and cysts that arise in the disease:
- Type 1 – pheochromocytoma is not present in the patient
- Type 2 – pheochromocytoma is present in the patient
o Type 2A: Pheochromocytoma with CNS hemangioblastomas
o Type 2B: Pheochromocytoma with both CNS hemangioblastomas and RCC.
o Type 2C: Pheochromocytoma is present without any other tumor types.
Your doctor will discuss the treatment options that are available for the tumors and cysts that are present as symptoms of your VHL gene alteration, as it is impossible to predict where and when a tumor may grow or how the disease progresses.
Who Treats Von Hippel-Lindau Disease and Tumors
The treatment and management of VHL require a multidisciplinary team that is generally centered around the primary care provider. The involvement of other specialists, such as neurologists, oncologists, ophthalmologists, and pediatricians, is dependent on the type of symptoms or the patients' need for specific treatments and assessments.
Members of the multidisciplinary team of specialists to treat VHL may include:
Primary care provider they provide referrals to specialists based on any new or existing symptoms that you may have. The primary care provider is any doctor practicing general medicine, pediatrics (for children), obstetrics/gynecology, or family medicine. A patient’s primary plays an essential role in the care of the patient as they coordinate and help manage the patient’s overall medical care.
Pediatricians These doctors specialize in the care of children (from birth to young adulthood) and can care for children who have been diagnosed with diseases such as VHL.
Geneticists are medical professionals that specialize in the diagnosing, treating, counseling, and management of people who are at risk or have a disease caused by a genetic disorder. Geneticists can also provide genetic counseling to patients.
Ophthalmologists These are doctors that specialize in both surgical and medical care of patients who have diseases affecting the eye. Ophthalmologists diagnose, treat, and manage.
An oncologist- Is a doctor that specializes in the diagnosis, management, and treatment of cancers and benign and malignant tumors.
Neurologist- Specializes in the diagnosis, treatment, and management of impaired function and diseases of the nervous system. The muscles and blood vessels that are related to the nervous system are also cared for by the neurologist.
Nephrologist specializes in diseases that affect the kidneys, fluid and mineral balance, and blood pressure.
Endocrinologist specializes in diseases associated with glands, metabolism, and hormones.
How is Von Hippel-Lindau (VHL) disease Diagnosed?
As VHL is a genetic disease, genetic testing via a blood sample (from the vein or a finger prick) is the most conclusive way to diagnose someone with the disease. The majority of people who have a genetic mutation in their VHL gene will be confirmed to VHL once being tested.
There are no specific guidelines in terms of who has to be tested for VHL. According to Dr.Else, testing for VHL should also be done for the following groups of people:
- Patients that have a strong family history of kidney cancer or there has been more than one kidney cancer in the same family member.
- "Pretty much everybody" who has a hemangioblast of the brain or of the retina (eye).
- Patients that have pheochromocytoma a type of neuroendocrine tumor that arises from chromaffin cells (found in the adrenal glands).
A list of suggested VHL Referral criteria for patients can be accessed here.
What Treatments Options are Available
VHL is an incurable disease, with the goal of treatment to suppress or remove tumors before they become a problem. Dr.Rogers explains his initial steps for when a patient is suspected of or has been diagnosed with VHL. Treatment options for VHL vary significantly due to all the possible manifestations of the disease that may occur in an individual patient. Multidisciplinary medical teams are thus essential to provide the appropriate care for someone diagnosed with VHL. Treatment options could range from immediately needing to remove a patient's single tumor or monitoring a patient that presents with multiple tumors in different parts of the body.
Your doctor will be able to determine the best treatment option for the removal of your tumors by:
- Surgery
- Laser therapy
- Cryotherapy (the application of extreme cold)
- Immunotherapy
- Targeted therapy
- Medication (such as Belzutifan)
If kidney cancer is present in a VHL patient, there is, according to Dr. Tobias Else, an endocrinologist who leads the comprehensive Clinical Care Center For VHL disease, a more "well defined" protocol to follow. When treating renal cell cancer (tumors), Dr. Tobias Else explains that they "tend to watch them until they approach the size of three centimeters. And that's when our [urologic] oncologist will do the surgery and remove those tumors…." Each case is different and requires an interdisciplinary team to provide the care needed.
Newer treatment options are becoming available; just last year (2021), the FDA approved the drug belzutifan for adult VHL patients that do not require immediate surgery. Belzutifan is only approved for the treatment of central nervous system (CNS) hemangioblasts, pancreatic neuroendocrine tumors (pNET), or associated renal cell carcinoma (RCC). There are side effects, as with many medications, and some considerations to take into account before deciding if this drug is for you.
Multidisciplinary medical teams are thus essential to provide the appropriate care for someone diagnosed with VHL.
How can Von Hippel-Lindau Disease and Tumors be Prevented?
To prevent new complications and tumors from developing in patients with VHL, continual lifelong monitoring is needed for the rest of their lives. Screening and testing are recommended to occur yearly, once every second year, or every time a new symptom presents.
Von Hippel-Lindau screening and testing procedure:
- Eye examination to screen for retinal hemangiomas.
- Imaging -MRI of the brain and spine to screen for tumors. Ultrasonography or MRI of the abdomen to screen for pancreas tumors, pheochromocytomas, and kidney cancer.
- Hearing tests to screen for endolymphatic sac tumors in the inner ear
- Blood tests and blood pressure tests are used to screen for pheochromocytomas.
- A physical examination
What are the Risk Factors for Von Hippel-Lindau Disease and Tumors
There is no definitive way to predict which tumor will present in individuals and how severe the tumor will be, even if the same VHL genetic mutation is present in a family.
The estimated risk factors for those with VHL developing certain tumors include:
- About 70% of VHL patients present with hemangioblasts of the CNS.
o 44-72% of hemangioblasts are found in the cerebellum
o 13-50%of hemangioblasts are found in the spinal cord
o 10-25% of hemangioblasts are found in the brain stem
- About 60% of cases are retinal hemangioblasts
- 25-60% of cases present with Kidney cancer or clear renal cell carcinomas
- 9-17% of cases present with Pancreatic neuroendocrine tumors
- 10-25% of cases present with endolymphatic sac tumors
- 10-20% of cases present with pheochromocytomas or paragangliomas
Aftercare Consideration of Von Hippel-Lindau Disease and Tumors
Even though there is no cure for VHL, patients can still live a full life, through effective management, of their condition and by reducing the impacts that the symptoms of the tumors may have. As VHL symptoms can present throughout life, ongoing monitoring, such as screening for new tumors (active surveillance)
Effective management of VHL includes the following considerations:
- Depends on the specific diagnosis and type of severity of associated symptoms in the individual.
- An interprofessional healthcare team is needed to address the multiple and varying manifestations of the disease.
- Lifelong monitoring
- Family members need surveillance and screening
- Annual blood
- Imaging (e.g,. MRIs)
- Genetic counseling and testing
VHL Alliance provides a comprehensive list of different support options to help you deal with the emotional toll that this disease has. Support groups not only cater to the patient but also to the family affected by this genetic disease.
Questions To Ask Your Doctor
- Should I be concerned that I can get tumors elsewhere in my body?
- What are my treatment options?
- What does my surveillance plan look like?
- What can I do to reduce my risk of getting cancer?
- How are my tumors going to affect my daily life?
- Should I consider genetic testing?
Learn more about SurvivorNet's rigorous medical review process.