FDA Requiring Women Be Told About Their Breast Density During Mammograms
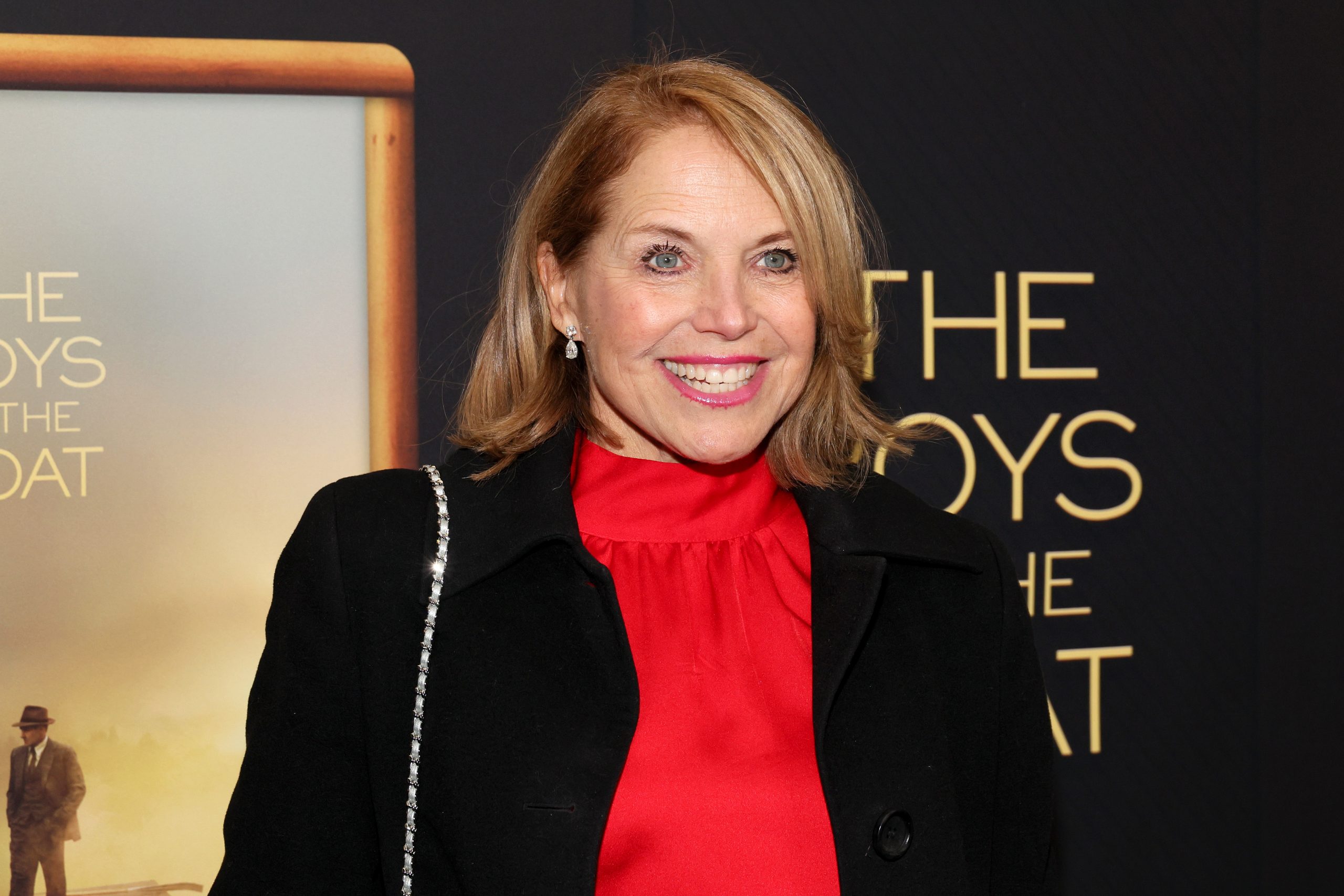
- Journalist Katie Couric, 67, is a breast cancer advocate who emphasizes the extra steps needed for women with dense breasts when screening for cancer. Couric was diagnosed with breast cancer in 2022, and she later learned she has dense breasts.
- Dense breasts mean there is more fibroglandular tissue and less fatty breast tissue.
- The Food and Drug Administration (FDA) now requires mammogram reports to include a section that informs women about their breast density.
- Women with dense breasts are at a higher risk for developing breast cancer because dense breast tissue can mask potential cancer during screening.
- While mammograms are extremely valuable for breast cancer screening, more effective screening methods exist for women with dense breasts.
- 3D mammograms, breast ultrasound, breast MRI, and molecular breast imaging are options for women with dense breasts for a more precise screening. It is important to ask your doctor about your breast density and cancer risk.
Journalist Katie Couric, 67, is among the most passionate breast cancer advocates in media, and this is particularly true when discussing dense breasts. Couric has dense breasts, which means she has more fibroglandular tissue and less fatty breast tissue. During mammograms, the tissue difference can make locating signs of cancer more difficult in women with dense breasts.
Now, the Food and Drug Administration (FDA) is requiring women undergoing mammograms, which screen for breast cancer, to be notified of their breast density.

- “The breasts are almost entirely fatty.”
- “There are scattered areas of fibroglandular density.”
- “The breasts are heterogeneously dense, which may obscure small masses.”
- “The breasts are extremely dense, which lowers the sensitivity of mammography.”
Understanding Your Mammogram Report and Breast Density
A radiologist reading mammograms categorizes breasts into four different categories using the Breast Imaging Reporting and Data System (BI-RADS), a classification system developed by the American College of Radiology (ACR). These include:
- Fatty breast tissue: These breasts are mainly composed of fat with very little dense tissue. Found in less than 10% of women, fatty breasts appear dark on mammograms.
- Scattered fibroglandular breast tissue: These breasts contain a mix of fatty and dense tissue (composed of glands and fibrous tissue). On a mammogram, they have dark areas (fatty tissue) intermixed with light areas (dense tissue). Around 40% of women have breasts that fall in this category.
- Heterogeneously dense breast tissue: This type of breast tissue has many areas of dense tissue and some areas of fat. Found in 40% of women, these breasts look mostly light, with some dark areas on a mammogram.
- Extremely dense breast tissue: Such breasts are almost entirely composed of dense glandular and fibrous connective tissues with very little fat. They are found in 10% of women and appear light on mammograms.
Your breasts are usually called dense on a mammogram report if they fall within the heterogeneously dense breast tissue or the extremely dense breast tissue categories.
WATCH: When You’re Getting a Mammogram, Ask About Dense Breasts
Couric was diagnosed in June 2022 but revealed her cancer to the world during Breast Cancer Awareness Month last year. She was diagnosed with early-stage breast cancer, specifically stage 1A.
“I was nervous about it. I waited a few days so I could process it and really understand what we were dealing with,” Couric said to “Today” at the time.
Dr. Michael Zeidman, assistant professor of surgery at Icahn School of Medicine at Mount Sinai in New York City, tells SurvivorNet that stage 1 is divided into two subcategories, 1a and 1b. Stage 1a breast cancer means the cancer hasn’t spread outside the breast. Stage 1b means there’s no tumor in the breast; instead, small groups of cancer cells are found in the lymph nodes. Stage 1b can also mean there’s a tumor in the breast and small groups of cancer cells in the lymph nodes. Stage 1 also means the cancer was caught very early, he says.
She underwent surgery and radiation therapy to treat the cancer a few months after her diagnosis.
During Couric’s cancer journey, she learned she had dense breasts. To help her navigate the challenges dense breast tissue brings during mammograms, Couric receives additional screening, which includes a breast ultrasound.
Additional screening methods are helpful for women with dense breasts because glandular tissue appears white on mammograms. Cancer and other abnormalities also exhibit a similar appearance. The “frosted glass” effect from the glandular tissue can thus mask cancerous areas, especially nascent ones. Undetected, these cancers can progress, growing large and advanced. They will then likely require more intensive treatments to cure or can become incurable altogether.
RELATED: Millions of Women With Dense Breasts: A New Congressional Law What You Need to Know
Helping Patients Better Understand Dense Breasts
- How to Avoid False Positive Cancer Results in Women With Dense Breasts: Ultrasounds Used in Addition To Mammograms
- I Have Dense Breasts. Do I Need a 3D Mammogram?
- Millions of Women With Dense Breasts — A New Congressional Law — What You Need to Know
- When You’re Getting a Mammogram, Ask About Dense Breasts
Enhanced Screening for Dense Breasts
Women with dense breasts may not know they have it based on feeling alone. Breast density is determined by its appearance on a mammogram. Dr. Connie Lehman, the chief of the Breast Imaging Division at Massachusetts General Hospital, explains to SurvivorNet that fatty breast tissue appears gray on an X-ray. Conversely, dense breast structures appear white during an X-ray. Cancers also appear white on an X-ray, meaning the dense breast structures can mask the possibility of cancer. Luckily, advanced mammograms exist to help doctors navigate this obstacle.
WATCH: 3D Mammograms explained.
“Digital mammography, it turns out, significantly improves the quality of the mammogram…It’s 3D or tomosynthesis mammography,” Dr. Lehman explains.
“This allows us to find more cancers and to significantly reduce our false-positive rate. With digital mammography 3D tomosynthesis, we’re taking thin slices through that breast tissue, like slices of a loaf of bread. We can look at each slice independently rather than trying to see through the entire thickness of the entire loaf of bread. So those thin slices help us find things that were hidden in all the multiple layers,” Dr. Lehman adds.
Additional testing can be considered for dense breasts, depending on a woman’s personal history, preferences, and her physician’s guidance. These tests include:
- 3-D Mammogram (Breast Tomosynthesis): This technology acquires breast imaging from multiple angles and digitally combines them into a 3D representation of the breast tissue. This allows physicians to see breast tissue architecture better, even in dense breasts. 3D mammograms are fast becoming the standard way of performing mammography.
- Breast Magnetic Resonance Imaging (MRI): An MRI machine uses magnets to create highly detailed, intricate images of the breast. These are mostly reserved for women with an extremely high breast cancer risk. Dense breasts alone may not be a valid reason to obtain a breast MRI. However, dense breasts in women with genetic mutations, like BRCA1 and BRCA2, or a strong family history of breast cancer could justify obtaining breast MRIs.
- Molecular Breast Imaging (MBI): MBI is a newer imaging technique that uses a radioactive tracer to detect breast cancer. It is beneficial for women with dense breasts. However, MBI is not as widely available as other screening methods.
A new rule from the Food and Drug Administration (FDA) says that facilities offering mammograms must notify patients about their breast tissue density and recommend they speak with a doctor to determine if further screening is necessary. There will be “uniform guidance” on what language to use and what details to share with the patient to make the communication clear and understandable.
Breast Density Doesn’t Remain the Same Over Time, Impacting Your Cancer Risk
Women with dense breasts are at a higher risk for developing breast cancer. This connection has been demonstrated time and again in several rigorous scientific studies. 1 in 6 women with dense breasts are at risk for breast cancer. Comparatively, 1 in 8 women with average breasts are at risk for this cancer. The exact reason for this difference is not fully understood.
Researchers from Washington University School of Medicine in St. Louis and Brigham and Women’s Hospital in Boston analyzed this connection in a new study.
They recruited 947 women between November 2008 and October 2020. All women were cancer-free at the start of the study and received yearly or bi-yearly screening mammograms. Researchers tracked the women’s mammogram reports and breast densities over time.
All women experienced a decline in their breast density during the 12 years. Two hundred eighty-nine women developed breast cancer during this time. Those who developed cancer had a lower rate of decrease in breast density than those who did not. The researchers concluded that the rate of breast density changes may indicate future breast cancer risk.
What To Ask Your Doctor
If you have been diagnosed with breast cancer, you may have questions about keeping your strength through treatment. Here are a few questions to help you begin the conversation with your doctor:
- What treatment will I be receiving?
- What side effects are associated with this treatment?
- Are there steps I can take daily to help minimize these side effects?
- What physical activity routine do you recommend for me during treatment?
- Do you have recommendations for someone who doesn’t particularly enjoy exercise?
- Can you recommend a dietician who can help me with healthy eating tips and weight maintenance?
- I’ve been having trouble sleeping. Do you have any treatment recommendations?
Learn more about SurvivorNet's rigorous medical review process.

