Psoriasis (pronounced sor-EYE-a-sis) is a skin condition that causes red, itchy patches to develop on the skin. For people living with this disease, symptoms can be uncomfortable and sometimes embarrassing.
Unfortunately, psoriasis does not have a cure, but the good news is that symptoms can often be managed with different treatments and some lifestyle adjustments.
Read More1. How do you get psoriasis?
The specific cause of psoriasis is unknown, though the condition is thought to be caused by skin cells that are growing abnormally faster than other cells. Since the skin cells are multiplying so quicklyup to 10 times faster than normalthis makes the skin shed every few days.Like most auto-immune diseases, psoriasis outbreaks may be triggered by stress or injury, sunburn, medication, another illness or infection, tobacco and/or alcohol. Cold and dry weather can also affect people with psoriasis as it dries out the skin. Sometimes there is no rhyme or reason to the level of severity with each flare-up of psoriasis, which is known to be hereditary, meaning the condition can run in your family.
2. What are the first signs and symptoms for psoriasis?
Like some types of viruses, psoriasis is often asymptomatic, or symptomless, so people who have the disease will not be dealing with constant outbreaks.
"Some patients report itching [or a] burning sensation, but that doesn't tend to be the norm. It certainly can happen," Dr. Khattri explains. "Then if you have psoriasis in the genital area, it can feel uncomfortable just because it's in a very sensitive part of the body. But for the most part, it tends to be asymptomatic."
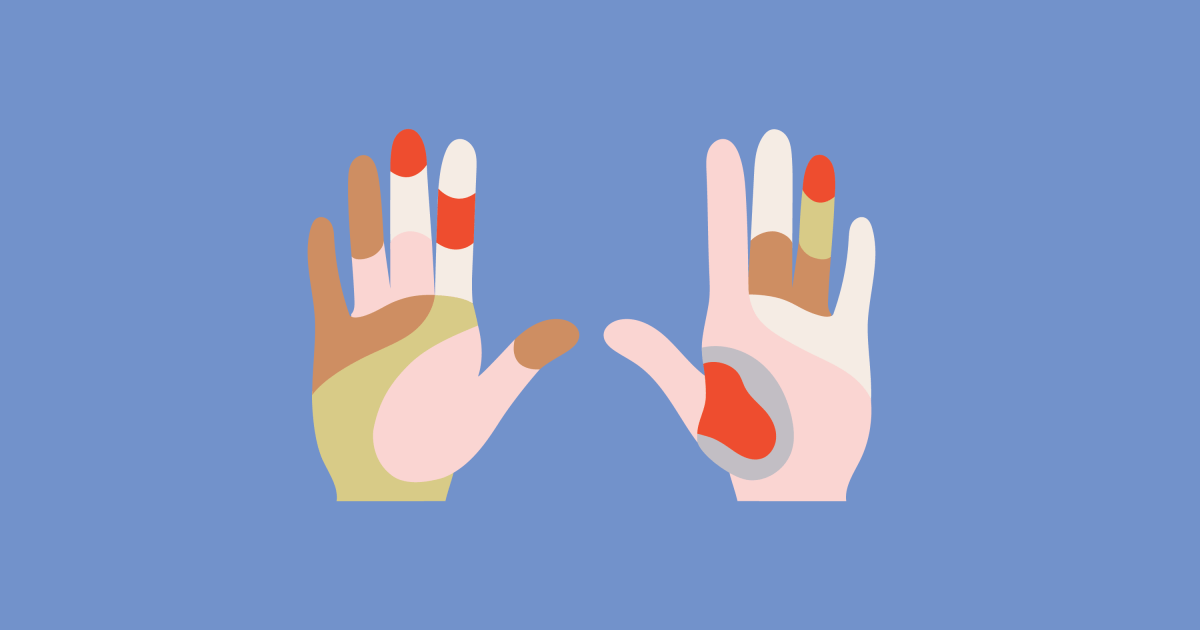
Dr. Khattri recommends seeing a dermatologist if you notice red, scaly spots on the body so a doctor can make a proper diagnosis. Psoriasis patches can vary in how they appear on the skin. The disease may present as just a few spots with dandruff-like scaling or as rashes that cover large parts of the body. The most commonly affected areas are the lower back, elbows, knees, legs, soles of feet, scalp, face, and palms.
Dr. Khattri describes clinical symptoms of psoriasis
We also spoke with Dr. George Han, a dermatologist at Northwell Health/Lenox Hill Hospital, who says he sees many patients with itching.
"It's interesting because if you look at the older dermatology textbooks, there was this concept that psoriasis is not supposed to itch,” he says. “And so they made this distinction between the itchy rash, which is eczema dermatitis and psoriasis, which is supposed to be not itchy, but if you actually ask patients and in some of the literature now, upwards of 80, 90% of patients do have itching associated with psoriasis."
Along with itchiness or scaly, red spots, other reported symptoms associated with the disease often include:
- Red patches of skin covered with silvery scales
- Small scaling spots
- Dry, cracked skin that may bleed or itch
- Burning, or soreness
- Thickened or ridged nails
- Swollen or stiff joints
Dr. Han says most types of psoriasis can be diagnosed clinically, meaning the doctor can determine psoriasis just by viewing the affected area or areas. With more atypical forms of psoriasis, a biopsy may be needed.
3. What areas of the body are most affected by psoriasis?
A rash from psoriasis can really show up anywhere. Fortunately, in most cases, psoriasis only develops on a few patches of skin. However, in severe cases, the plaques connect and cover more surface area of the body. “Plaques” specifically refer to the raised red patches covered with a white-colored buildup of scales, or abundance of dead skin cells.
Psoriasis can be very agitating, causing you discomfort. In addition to the physical itchiness, it can make you self-conscious. In general, psoriasis tends to affect the:
- Elbows and knees.
- Face, scalp and inside the mouth.
- Fingernails and toenails.
- Genitals.
- Lower back.
- Palms and feet
4. What are the different types of psoriasis?
There are seven different types of psoriasis, with plaque psoriasis being the most common. The types differ in how they present and what they are caused by.
- Plaque psoriasis: This is the most common form of the disease and causes dry, raised skin patches that may be covered in scales. The patches may be itchy and tender.
- Nail psoriasis: This disease can affect fingernails and toenails and might cause nails to loosen from the nail bed.
- Guttate psoriasis: This disease typically affects young adults and children and is often caused by a bacterial infection like strep throat.
- Inverse psoriasis: This type of psoriasis mainly affects skin folds, so it will often present in areas such as the groin, buttocks, or breasts, and can worsen with friction or sweating.
- Pustular psoriasis: This is a rare form of psoriasis that causes pus-filled blisters to develop in widespread patches across the body.
- Erythrodermic psoriasis: This is also a rare form of the disease. It can cover the entire body with a red, peeling rash that may itch or burn intensely.
- Psoriatic arthritis: With this form of the disease, joints may become swollen and painful. Sometimes, joint pain is the first or only symptom, while other times other symptoms like nail changes will occur.
Dr. Khattri explains the different types of psoriasis
5. How is psoriasis managed?
Psoriasis is a chronic disease that does not have a cure, but symptoms can often be managed with different treatments and some lifestyle adjustments. Treatment options basically fall into three categories: topical treatments (which would be ointments or creams you can rub on the skin), phototherapy (using UVB light to treat the disease), or systemic treatments (drugs taken either orally or through an IV that treat symptoms by targeting parts of the immune system).
Topical Treatments
Topicals are considered a mainstay for treating psoriasis, and there are several different options available. When it comes to topicals, the route you go with will depend on what type of psoriasis you have and how symptoms are presenting. For more severe cases, topical treatments aren’t effective enough, but it’s a good starting point to try to get the condition under control.
Some of the different topical creams and ointments that may be prescribed include:
- Corticosteroids: These drugs may be prescribed to treat mild to moderate psoriasis and can be a good option during flare ups. They are available as ointments, creams, lotions, gels, foams, sprays, and shampoos. Topical corticosteroids are classified into seven categories based on their potency, ranging in strength from ultra-high to low. Lower potency corticosteroids are typically used on the face, while areas with thick, chronic plaques often require treatment with ultrahigh-potency corticosteroids.
- Vitamin D analogues: These synthetic forms of vitamin D can help slow skin growth. The drugs can be used alone or in combination with corticosteroids. Calcipotriene (also known as calcipotriol) and calcitriol are the two commonly used synthetic vitamin D analogues.
- Retinoids: Retinoids can come as a gel or cream and be used to relieve some psoriasis symptoms. Topical tazarotene can be particularly helpful for palmar-plantar psoriasis (palms and soles) and nail psoriasis, the AAD and NPF guidelines say.
- Calcineurin inhibitors: These drugs reduce inflammation and plaque buildup. These may be helpful in areas where skin is thin, like around the eyes, but should not be used for long periods of time due to potential side effects. Although not FDA approved for psoriasis, the topical calcineurin inhibitors tacrolimus and pimecrolimus are often used in the treatment of psoriasis.
- Salicylic acid: These shampoos and scalp solutions can reduce the symptoms of psoriasis on the scalp. Salicylic acid minimizes scaling and softens plaques. It can also be combined with other topical medications including corticosteroids.
- Coal tar: A product of coal, this medication has been used to treat psoriasis for more than a century, according to AAD and NPF. These drugs can reduce scaling, itching, and inflammation and can be included in shampoos, creams, and oils.
Phototherapy - Another treatment option for psoriasis is phototherapy. This therapy is generally used when medications applied to the skin alone do not work and alternative options are needed. It can also be used for patients who wish to avoid medications that can affect their entire body (system medications). Phototherapy can also be used in conjunction with topical and/or systemic psoriasis treatments.
Phototherapy exposes patients with psoriasis to narrow band UVB light.
"It's a limited spectrum of the sunlight, which we use. Patients generally have to come to a place that does phototherapy. There's a phototherapy box. You go there. It's generally three times a week in the very beginning until your psoriasis is in control. And beyond that we can space it apart to once a week or twice a week as maintenance," Dr. Khattri says.
A frequency of twice or three times weekly is effective and is recommended, according to the American Academy of Dermatology (AAD) and National Psoriasis Foundation (NPF) guidelines.
Systemic Treatment
As mentioned, sometimes treatments applied to the skin’s surface just aren't enough to clear stubborn psoriasis. That's where systemic treatment treatment that travels through your entire body rather than being aimed at one area can be beneficial for patients. Systemic treatments are available via oral medication and injections. Some have been around for decades, while others are relatively new to the landscape.
"I have patients who come in after having been to many other medical practices and not really getting much hope or really good treatments for their psoriasis," Dr. Han tells SurvivorNet. "And we'll give the patient a systemic medicine that these days are very effective. We have treatments where over half of the patients who have moderate to severe psoriasis are getting 100% clear."
Related: Injectable Treatments for Psoriasis: How Do They Work?
Systemic treatments may include oral medications like methotrexate, Apremilast (otezla), or cyclosporine. Biologic drugs, or biologics, which are given by injection or intravenous (IV) infusion (a slow drip of medicine into your vein), may also be given. These drugs target only specific parts of the immune system, while other systemic drugs target the whole system.
There are three main categories of biologics used to treat psoriasis, according to Dr. Khattri. These include:
- Injections that target and block TNF, a pro-inflammatory molecule that the body may be producing too much of when a person has psoriasis (includes drugs like Humira, Cimzia, and Enbrel)
- Injections that target and block IL-17, another pro-inflammatory molecule that could trigger psoriasis symptoms (includes drugs like Cosentyx, Taltz, and Siliq)
- Injections that target IL-12 or IL-23, which are also proteins linked to psoriasis symptoms (examples of these drugs include Tremfya and Ilumya)
"All of these are injections which are approved for psoriasis, and some of them are also approved for psoriatic arthritis," Dr. Khattri explains.
One patient we spoke with, who prefers to go unnamed, has had nearly 100% relief from using the drug STELARA (ustekinumab), which treats plaque psoriasis.
“I get a shot once every three months,” he tells SurvivorNet. “If my skin is a mess, takes about two weeks to work. It works different for everyone. For me, it almost completely clears me up. I started taking it in 2018, injecting it every three months. It’s a miracle drug. After taking it, it's like psoriasis doesn’t exist.”
Although this specific shot alarmingly costs $9,000 out of pocket, with certain insurance plans, the co-pay is $5.00.
“For the people who can't afford it or don’t have insurance, it sucks. If other, more affordable avenues don’t work, they have to continue living with it, which is messed up,” the patient says. “It's always there, you're always irritated, you're embarrassed.”
6. How can I help my psoriasis condition naturally?
Since psoriasis is known as an autoimmune disease, which is typically an inflammatory condition where the body mistakenly attacks your own cells, there are certain natural lifestyle changes that you can incorporate that won’t put as much stress on the body. In turn, the flare ups may diminish, or clear up completely for the lucky ones.
“Naturally, humidity and the sun work for me,” a psoriasis patient tells us. “This [condition] popped up when I was 35. As I got older is when it slowly started appearing; on my elbows, my legs, my scalplittle by little I was a mess. And nobody in my family has it,” he adds.
For some, the sun will exacerbate symptoms. Salt water from the ocean, however, can be good for clearing up skin conditions.
Also, eating an anti-inflammatory diet can reportedly help immensely for controlling flare-ups.
Some people with psoriasis try to combat its distressing effects by following a paleo diet.
A paleo diet, by definition, mainly consists of meat, fish, vegetables, and fruit, and excludes dairy or grain products and processed food.
According to the Paleo Diet website, “Foods that cause inflammation include refined carbohydrates, wheat and other cereal grains, soda and other sugar-sweetened beverages, margarine, shortening and lard, and processed meats.”
These types of foods can cause insulin (a hormone that controls our blood sugar) to spike in our bodies, which can contribute to inflammation and also alter our gut health, meaning change the ration of good bacteria vs. bad bacteria, which can wreak havoc on the body.
Overall, getting an adequate amount of rest and 7-8 hours of sleep every night is a tried and true method of putting less stress on your body, therefore lessening the severity of certain conditions like psoriasis.
7. Is psoriasis contagious?
Psoriasis is not contagious, but as mentioned, it is known to be genetic. It is common for people with psoriasis to feel physically unattractive with the condition, which is understandable, but with a supportive, loving partner who you can communicate with, it can hopefully make you feel better about yourself, and less self-conscious about your loved ones seeing or touching the affected areas on your skin.
8. How Will This Skin Condition Affect My Dating and Sex Life?
As with any conditions or diseases, like cancer, or sexually transmitted viruses like herpes, you often know you are with the right person when they are understanding and supportive of what you are going through, and work to help you find solutions to manage physical and emotional drawbacks for dealing with your specific health issue.
Furthermore, it's important to note that “it's completely normal to feel nervous about having psoriasis, especially when it comes to intimacy,” Dr. Saakshi Khattri tells SurvivorNet. Dr. Khattri is understandably well-versed in this area, as she frequently counsels patients about this all-too-common concern.
When asked if he had any tips for psoriasis patients who may be nervous or stressed out about their condition when it comes to their dating and sex life, Dr. Khattri offered some words of wisdom. "It's OK to feel nervous about having psoriasis," Dr. Khattri says. "It's OK to feel overwhelmed."
Related: 'I'm Single and Have Psoriasis. How Does This Affect My Dating Life? What About Sex?'
Dr. Han weighs in on this important topic as well, as it is primarily a chief concern with patients.
"People have come in with inverse psoriasis (a form of psoriasis that occurs in areas where the skin folds), even without psoriasis elsewhere," he says.
This means patients have painful inflammation in their private areas, "and it's very embarrassing," which is understandable. "They don't really want to talk about it," he adds, which can make it especially hard on a person's dating and sex life.
"So it's important that we diagnose it (the psoriasis) correctly and help counsel the patients," Dr. Han explains.
Counseling patients can include explaining how to talk with potential sexual partners about psoriasis, especially if you're experiencing inflammation in your genital region. Make sure to your doctor for further assistance.
9. Can Psoriasis Predispose You to Other Illnesses Like Covid-19?
Psoriasis is somewhat rare, and treatment can vary quite a bit from patient to patient. Some people may be able to make simple lifestyle adjustments, while others will need medical interventions. The disease has also been linked to several other ailments. It increases the risk of developing diseases such as psoriatic arthritis, inflammatory bowel disease, and others.
Related: Can Psoriasis Predispose You to Other Illnesses Like Covid-19?
With Covid-19 still spreading around the world, many people with psoriasis may be worried about the risks an infection would pose to them particularly because psoriasis is an autoimmune disease. According to research presented by the Keck School of Medicine at the 2021 virtual meeting of the American Academy of Dermatology, people with psoriasis were more likely to contract Covid-19 compared to the general population.
However, study authors noted that the patients with psoriasis were also more likely than the general population to have other Covid-19 risk factors, like congestive heart failure, type-2 diabetes mellitus, obesity, or chronic obstructive pulmonary disease. People with psoriasis may want to continue taking precautions against Covid-19 infections like avoiding crowded places, masking up, and regularly washing hands due to these findings.
Since Covid-19 is still a relatively new illness, there have been limited studies so far on how it affects people with psoriasis. There are, however, other illnesses with well-documented links to psoriasis.
"Psoriasis is an auto-immune disease, and…we say that if you have one auto-immune disease, it increases the risk of having other auto-immune diseases," Dr. Khattri tells us . "There are some auto-immune diseases that sort of cluster with psoriasis. Psoriatic arthritis is one of them; it's seen in about a third of patients that have psoriasis."
While everyone with psoriasis won't go on to develop an associated illness, it's still important to keep your doctor informed about any new symptoms you develop due to this increased risk.
10. How do I manage my feelings of embarrassment or shame with my psoriasis?
As a reminder, it's completely normal to feel nervous or continuously aware of your psoriasis, which can be difficult for many in their daily life. However, you may also be wondering how you can manage those feelings surrounding your psoriasis.
One piece of advice Dr. Khattri offers to manage this stress is advocating for yourself.
"If you have psoriasis on your skin, and if it's affecting your quality of life, it's important to advocate for yourself and not be dismissed by a health care practitioner," Dr. Khattri says. "And if you feel thiswherever you have psoriasis is really affecting you, just ask for options to treat your psoriasis."
With any condition, it can take time and patience to figure out best how to manage symptoms physically and emotionally. Just remember, you’re not alone, and there are resources and professionals out there who can help you.
Contributing by SurvivorNet staff.
Learn more about SurvivorNet's rigorous medical review process.